CASE STUDY
Innovative, Personalized Intranasal Flow Simluations
Dr. Krause used Materialise Mimics to simulate intranasal flow, illustrating every step of the process, from the segmentation of the flow region to the surface shape reconstruction and more.

Industry
Healthcare
Key solutions
Materialise Mimics
The impact
Workflow automation
Robust and accurate segmentation algorithms
Take a deep breath. Now, close your mouth and breathe out through your nose. What you have just done, expiration through your nasal cavity, is what is simulated in the following study. Every step of the process, from the segmentation of the flow region to the surface shape reconstruction and more, is illustrated by Dr. Krause’s Mimics Innovation Awards-winning study. The challenges faced during preprocessing, which arise from shapes so complex that modern CT scanners cannot capture them exactly, are met using Mimics in combination with an innovative automated grid generation and initialization concept.
“We appreciated Mimics’ user-friendly interface and the time it saved us. The graphical user interfaces and automated routines enabled a high-quality segmentation and reconstruction of the complete human nasal cavity. Furthermore, we found the segmentation algorithms to be both robust and accurate. Finally, 3-matic eased the process of reconstructing thin tissue that was only partly captured by the CT scanner,” says Dr. Krause, from the Karlsruhe Institute of Technology, Germany.
Turning CT data into a surface mesh with Mimics Core and 3-matic


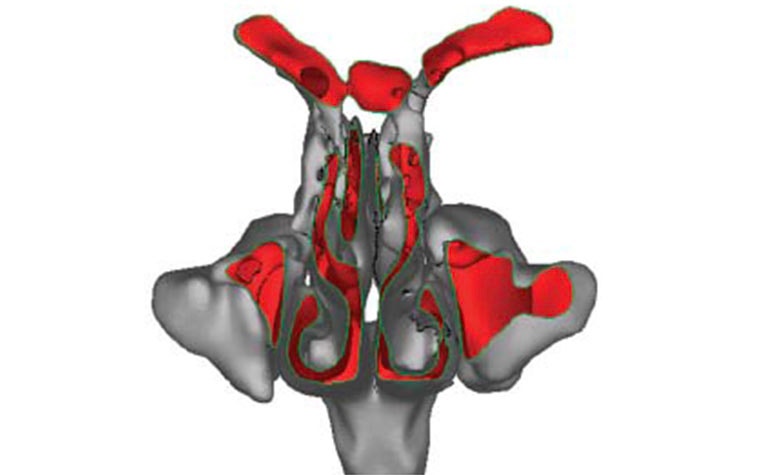
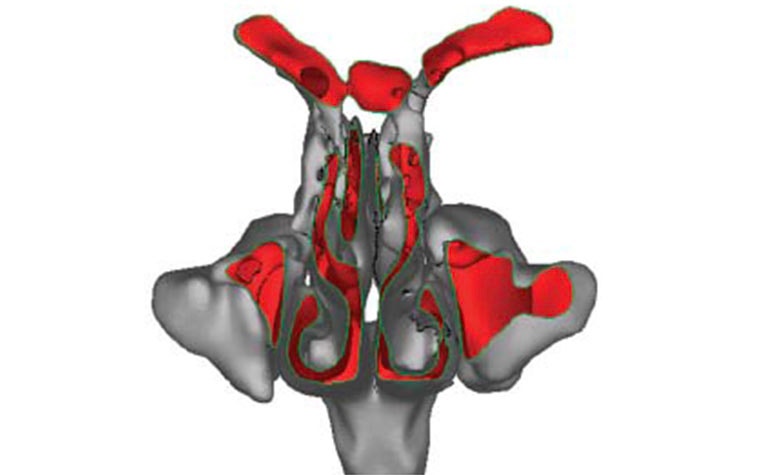
The construction of a surface mesh, based on CT data of the inner nasal cavity, is done in two main steps. First, the region of interest is segmented and represented as an STL surface mesh. Then, the unresolved fine structures, which are crucial for the flow characteristics, are reconstructed. For the first step, Dr. Krause applied seeded and dynamic region growing segmentation schemes. By doing so, he was able to identify the region of interest according to a defined color level or a special change.
Mimics Core proved ideal for accomplishing this step, and to a large extent, it automated the process. The second step, the reconstruction of unresolved structures like small air cavities, paranasal sinuses, and thin passages and tissues, was performed with the help of physicians, 3D visualization techniques, and 3-matic. For this study, the small tissue separating two passages could not be reconstructed completely. However, some captured parts of the tissue formed a needle structure in the segmented surface representation, so the problem could be solved using tools in 3-matic.
Preparing the simulation using a volume mesh
In order to simulate the airflow in the nasal cavity numerically, the volume needed to be parted into small cubes of equal size, also known as voxels. Their vertices, also called nodes, with their linking edges provide the volume mesh needed for the LBM computation. In order to generate this type of volume mesh from an STL surface mesh, Dr. Krause chose the open-source Common Versatile Multi-purpose Library for C++, the code of which is included in the OpenLB library.
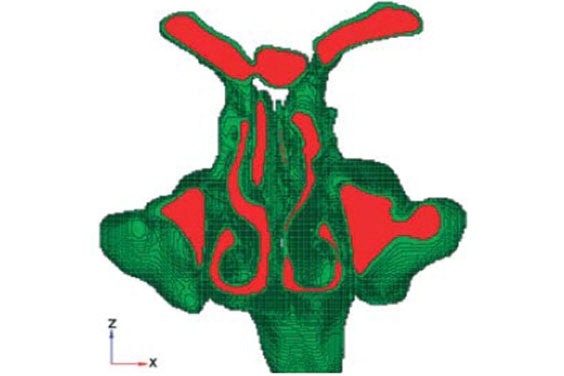

Before the airflow could be simulated on a computer, Dr. Krause needed to specify the inflow and outflow regions, which are located at the trachea and the two nostrils. He distinguished them from the flow region and the wall of the nasal cavity by assigning certain different material numbers to the nodes of the volume mesh. Depending on their distribution, it becomes possible to initialize the simulation algorithm. Yet, the initialization process for LBM algorithms and their automatization pose a challenge since the algorithm setup for each node depends on the material numbers of all neighboring nodes.
Furthermore, for particular material number distributions, the initialization is not possible. These difficulties were overcome by a generic concept proposed and realized in the OpenLB project. This concept relies on sophisticated routines that allow the original voxel mesh to be modified where needed without changing its characteristics.
Successfully simulating expiration and diagnosing a disorder
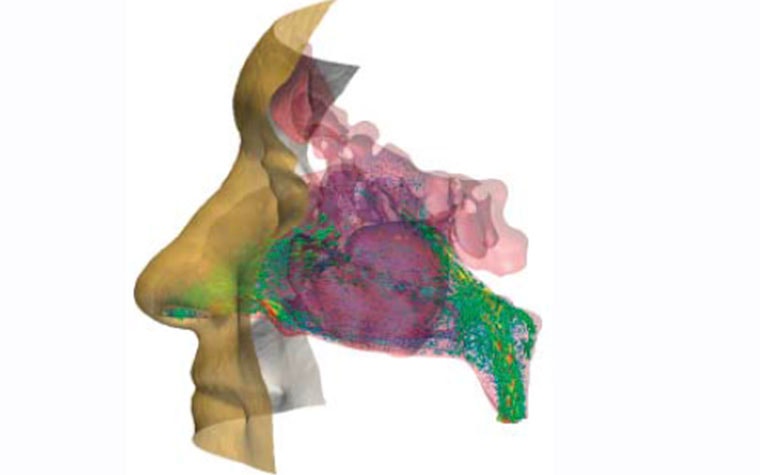
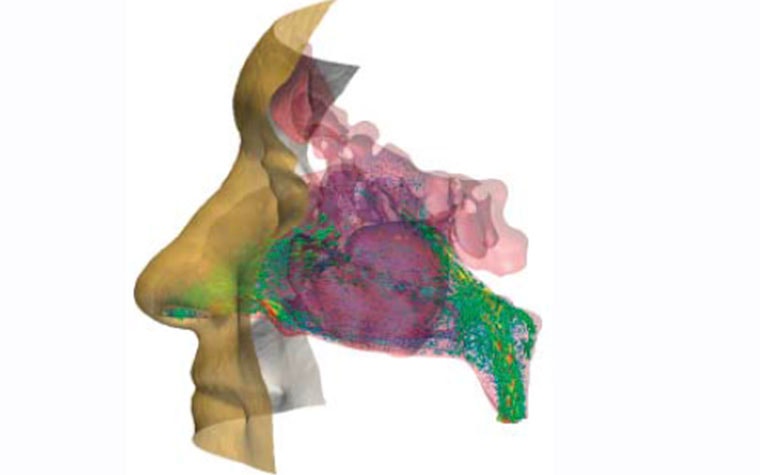
Expirations through the nasal cavity of a European male adult were successfully simulated with OpenLB. The results were validated by comparison with other experimentally and numerically gained results as well as with measurements taken from the patients involved. The visualized simulation results offer new insights into the flow characteristics of human respiration and, for one of the research subjects in particular, the personalized approach helped to locate a stenosis, which is now assumed to be the cause of a severe peripheral obstructive ventilation disorder that had been diagnosed before the study.
L-102833-01
Share on:
