EXPERT INSIGHT
How to Treat B2 Glenoid Cases

To spread the knowledge and experience of surgeons' use of medical 3D printing, and to illustrate how 3D planning can benefit your practice, we created a webinar series for 3D printing in orthopaedics. Here Dr. Carl Ekholm shares his presentation: “Complex Glenoids in my Practice."
Dr. Carl Ekholm is the head of the upper limb trauma and joint replacement unit of Sahlgrenska University Hospital and Associate Professor at the University of Göteborg, Sweden. In his webinar, he discusses how he used a glenoid implant instead of a bone graft to treat challenging cases of glenoid bone defect reconstruction.
The glenoid is the articulating surface on the shoulder blade. It occupies a humble volume of 10 cubic centimeters, roughly, a flat shot glass. It can easily get consumed by forms of arthritis or by unfortunate reactions to previous implants.
Classification methods and approaches
There are multiple defect classification tools available to determine the damage on the glenoid bone, and what approach to take. The solution is typically a combination of them. But there's no real consensus on which is best. Each case has to be evaluated and treated individually.
The Walch classification is one of the tools to determine the degree of bone erosion on the glenoid. Prof. Ekholm uses the Walch B2 glenoid to illustrate several treatment options to restore the joint. These include corrective reaming, oblique reaming, or structural grafting. Corrective and oblique reaming entail removing part of the bone, and result in altered mechanics in the shoulder. Structural grafting is another method, and aims at replenishing the bone stock and creating a fixation point stable enough to insert the standard implant. Personalized shoulder implants are another, yet relatively unexplored approach.
Currently, structural grafts with a glenoid implant are a popular choice. The difficulty however, lies in shaping the graft to fit perfectly into the glenoid. First, PMMA cement or bone wax is pushed into the glenoid to form a model. Then it is used as a template when sculpting the graft until there is a perfect surface match. Despite its common use however, corrective grafting still brings up issues in regards to grafting incorporation and why it does or does not succeed. The limit for the grafting technique is still uncertain.
When reaming and glenoid bone grafts are not enough
Some cases are beyond the limit of grafting. During the webinar, three such cases were discussed, two from Prof. Ekholm, and one from Dr. Wolf. All cases included the use of personalized implants using medical 3D printing. The first case was examined more extensively; a 72-year-old woman with rheumatoid arthritis with pain, and reduced range of motion (ROM).
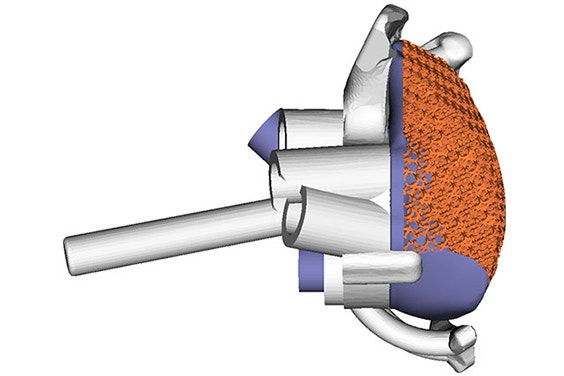
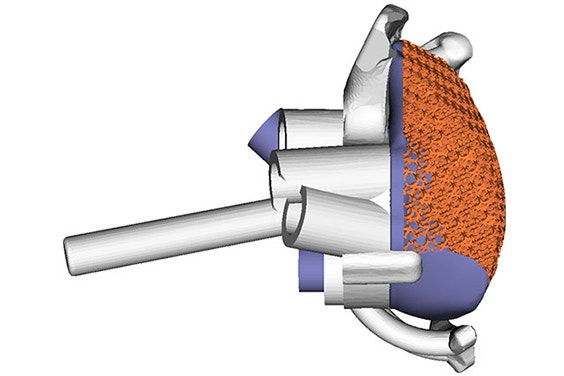
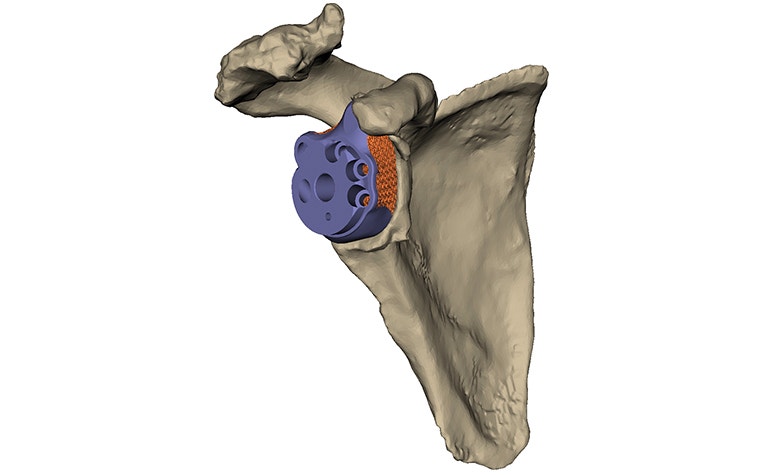
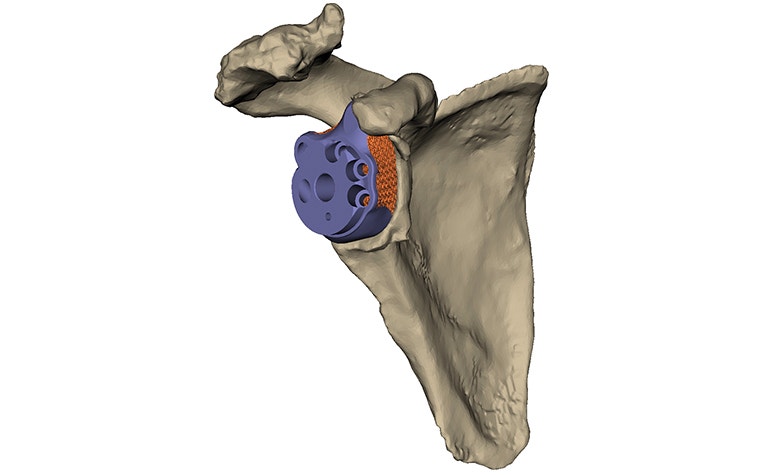
The case went as follows. Prof. Ekholm sent the CT scans to Materialise, and got a report back describing the anatomy, and an implant design. "It was extremely helpful in deciding what to do," says Prof. Ekholm. Loose bone fragments that would be removed during surgery, and what was left of the native glenoid, could easily be visualized. The scapula could be examined from different angles. A proposal for what implant could be used in this situation, and its positioning, was made. Finally, in the report, the surgeon could see where the implant was going to make contact with the glenoid, and where the plastic guide was going to make contact with the scapula, to guide the implant into its planned position. Prof. Ekholm and a Materialise clinical engineer held a virtual meeting with a shared screen to discuss modifications.
One year later, the patient is happy and pain free, with a reasonable ROM. Ultimately this is the goal of the surgery: for the patient to regain a reasonable ROM, and to reach a certain level of independence in regards to personal hygiene, cooking, eating, and basic household chores.
Another aspect of the case was assessing how well the surgery went and how the implant is still positioned. It's very difficult to do with CT scans alone. Prof. Ekholm was able to evaluate the outcomes more precisely by sending the one year post-op scans to Materialise for a post-operative report. He was able to view an analysis of how much deviation there was from the planned position of the implant and the screws.
The two other patients showed promise after their operations as well. Although there was slightly more deviation from the original positioning of the grafts and screws, the results were still satisfactory.
Promising 3D-printed implants
Because the technique is relatively new, personalized implants are more expensive than standard ones, and long-term results of glenoid reconstruction implants are not yet known. However, personalized implants are promising, according to Prof. Ekholm. The combination of careful planning and a personalized implant can provide perfect correction, and prevent the removal of very precious bone.
Although there's still a way to go, the future is keeping a spot open for a more common use of personalized implants. Currently, they are a promising option for difficult cases and a potential one for less complicated cases. Time and data will help in determining what happens next.


L-102971-01
Glenius is not yet commerically available in the US and Canada.
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
