INTERVIEW
Looking to the Future of TMJ Arthroplasty Surgery: How Personalized TMJ Implants Are Improving Surgical Success
In the evolving landscape of temporomandibular joint (TMJ) arthroplasty surgery, surgeons are embracing personalized solutions. 3D planning and personalized TMJ implants result in better patient outcomes by improving functionality and reducing chronic pain.
To delve deeper, we interviewed Dr. Laurence May, a CMF surgeon at Le Centre Hospitalier Universitaire Vaudois (CHUV) in Lausanne, Switzerland. Dr. May shares her experience with the Materialise TMJ Total Arthroplasty System. Not only does she shed light on the success she has achieved with these devices, but she also reveals the impact on her clinical practice.
Dr. May, you have used TMJ implants in your clinical routine. What would you describe as the main challenges when using a TMJ implant?
When it comes to utilizing TMJ implants in my clinical routine, I encounter several key challenges. First and foremost is accurately determining the appropriate indication for TMJ replacement. Additionally, ensuring effective patient communication and education is vital. However, perhaps the most intricate aspect lies in successfully transferring the virtual planning into the operating room. This entails skillfully navigating the delicate management of soft tissues, avoiding excessive tension that could lead to scarring, and precisely positioning the implant for optimal outcomes.
What are the main advantages of taking a patient-specific TMJ implant and a personalized approach with the support of a 3D-printed model? What is essential to consider before choosing a personalized solution?
The foremost advantage lies in the impeccable fit of the implant — it fits perfectly. This leads to enhanced stability. Additionally, this approach reduces operation time, which enables us to streamline procedures and achieve efficient outcomes. However, before opting for a personalized solution, it is essential to consider the costs and benefits involved carefully. Furthermore, the preoperative planning process can be time-consuming, and there may be potential production delays to consider. Balancing these factors is crucial when making the decision to embrace a personalized TMJ implant and personalized approach. This was not the case with Materialise as effective communication with the Clinical Engineer saved a lot of time.


You used a Materialise personalized TMJ implant for the first time during an operation in January 2023. Could you please describe your experience of using this implant?
Collaborating with Materialise as a new provider in this renowned field encouraged me to explore fresh perspectives regarding the materials and planning involved. The initial two cases yielded exceptional results, leaving both the patient and me satisfied. Encouraged by these successes, I am driven to further refine the workflow and advance our patient-specific approach.
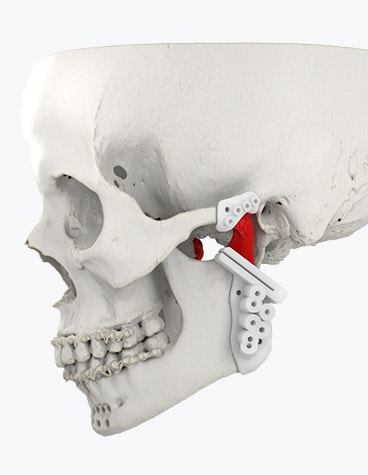
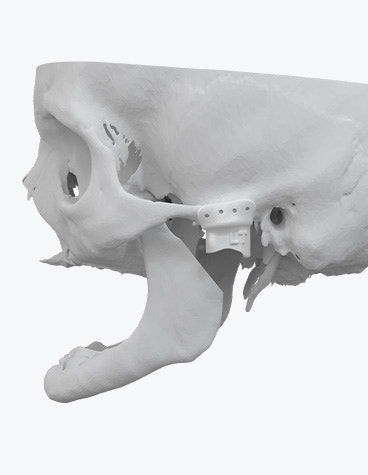

The Materialise TMJ Arthroplasty System consists of patient-matched guides, a polyamide trial implant, and a custom-made prosthesis.
Which surgical technique did you use for this procedure?
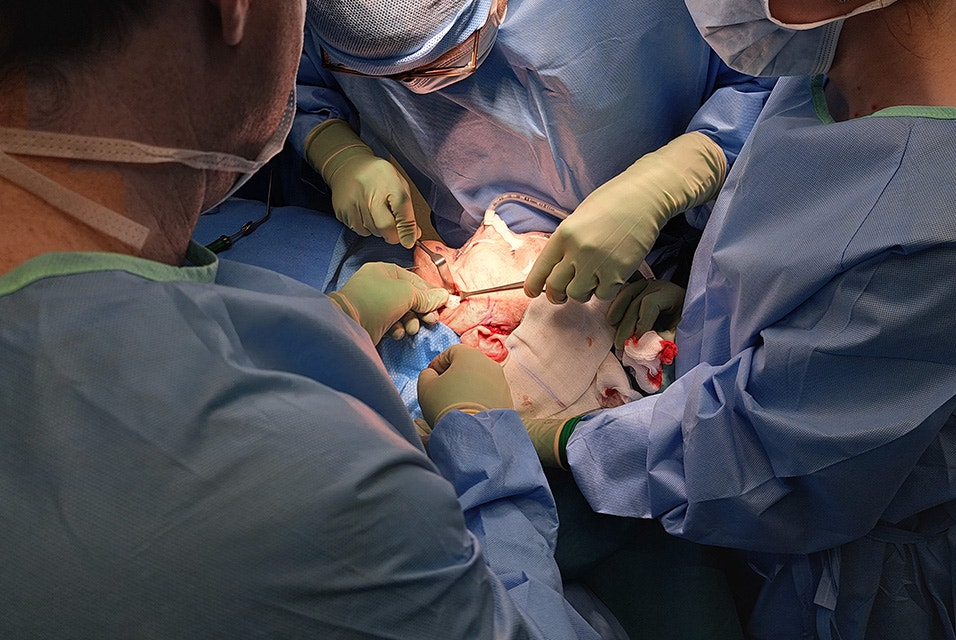
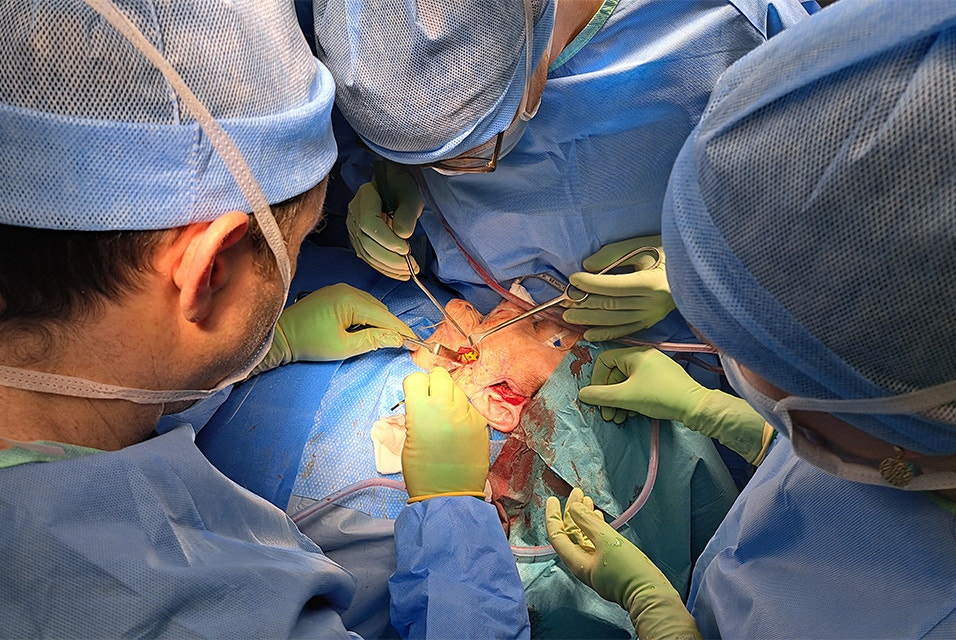
To insert and fixate the surgical guides and the TMJ prosthesis, two fixation sites need to be prepared which can be accessed by two surgical incisions. For this TMJ implant surgery, we employed a surgical technique that involved a submandibular approach in combination with a pre-auricular approach. A submandibular approach is used to expose the mandibular fixation site. The superior part of the mandibular fixation site can be accessed through the preauricular incision. Performing the mandibular osteotomy first creates more space to work on the temporal fixation site. After carefully making the necessary incisions, we prepared the implant site by removing the required soft tissues.
To ensure precise positioning, we utilized a mandible guide and then cut the condylar neck approximately 1 – 2 cm higher than the planned osteotomy. A unique aspect of our technique was first dividing the condylar head in half before its complete removal for greater freedom and accuracy during the final osteotomy.
Before removing the guide, we predrilled the holes and focused on completing the fossa component. With the fossa site fully prepared, we inserted the temporal trial implant, which fit flawlessly. We first fixed the fossa component with two screws and inserted the mandibular component via the submandibular incision and pushed the condylar head into the fossa of the temporal component. We fixed it with 2 screws as well. We conducted a thorough test to assess the functionality of the TMJ prosthesis and the rotation of the lower jaw, and, satisfied with the results, we proceeded to predrill and insert all remaining screws.
We concluded by closing the wounds and inserting two small drains since no coronoidectomy was required in this particular case. By employing this comprehensive surgical technique, we aimed to ensure optimal placement and functionality of the TMJ implant, ultimately enhancing the patient's quality of life and restoring their jaw's natural movement.
Meanwhile, you have used the Materialise TMJ implant for another case. What are the benefits you’ve seen from working with this implant and Materialise’s services?
Working with the Materialise TMJ implant and the services provided by Materialise has proven to be beneficial in several aspects. Firstly, the planning meetings with their clinical engineers have been exceptionally smooth and efficient. Their clinical expertise and preparedness instill confidence, eliminating the need for follow-ups or repeated requests. Secondly, the reliability of lead times allows for effective communication with patients, avoiding the common issue of constant rescheduling that often arises with other procedures. Lastly, the tactile sensation of the implant material is remarkably satisfying. I was really amazed at how well-produced they were and that they fit accurately, which makes them easy to use.
You mentioned the efficient support of Materialise’s clinical engineers; how was the collaboration with them during the planning session of the implant?
Effective communication is important when working with a team of clinical engineers. Their clinical expertise in understanding the patient's anatomy, including soft tissues, bone quality, and resection size, is essentially a game-changer. The support provided by these clinical engineers encompasses various aspects, such as their in-depth knowledge of the planning software, analysis of bone heat maps, discussions regarding optimal implant stabilization, and design of the implant. Furthermore, their experience working with other cases and surgeons greatly enriches the process. Even when my primary clinical engineer was unavailable, they effectively communicated my preferences to their colleague, ensuring continuity of service without any service gaps. I really enjoy working with my team!


In general, you are not only working with personalized TMJ solutions, but also with more personalized solutions for CMF procedures. To close this interview, which advice would you give to surgeons considering using personalized CMF solutions?
Firstly, it is crucial to have a solid foundation in traditional CMF procedures before embracing personalized solutions. While technology can enhance and streamline the process, it cannot replace the essential surgical skills and knowledge required. Secondly, meticulous consideration of the indication is of utmost importance. Carefully evaluate the patient's anatomy and the medical and financial benefits associated with personalized CMF solutions compared to conventional surgery. By combining expertise, technological advancements, and thoughtful patient selection, surgeons can harness the full potential of personalized CMF solutions for optimal outcomes.
L-103180-01
Share on:

Biography
Dr. Laurence May
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.