EXPERT INSIGHT
The Untapped Potential of Personalized Solutions for TMJ Arthroplasty

In 2022, surgeons performed 450,000 knee and hip replacements in Germany. In contrast, the number of temporomandibular joint (TMJ) replacements was nowhere near that figure. TMJ arthroplasty is more complex — it's associated with more risks and complications, and it requires a steeper learning curve for proper fitting. Despite these challenges, advancements in technology and proven outcomes from leading surgeons demonstrate that these operation numbers can successfully increase worldwide. With virtual planning and personalized surgical guides and implants, surgeons can improve precision and patient outcomes for TMJ arthroplasty.
Why is personalization the future of TMJ arthroplasty?
TMJ arthroplasty is a niche but critical solution, and personalized solutions can simplify these inherently complex procedures. It all starts with the plan. By virtually 3D planning based on patient images, surgeons can visualize the anatomy, map out resection lines, and design patient-specific implants and guides.
This advanced planning helps the surgeon prepare more efficiently and equips them with the tools for each unique surgery, minimizing unexpected intraoperative situations, and reducing procedure time. In a field like this, these added insights and specialized tools are crucial.
According to Dr. Daniel Thiem, CMF Specialist at the Johannes Gutenberg University of Mainz, "The biggest advantage of personalized TMJ implants is precision. Standard implants require significant intraoperative adjustments, which increases the procedure's complexity and introduces variability. Personalized implants, on the other hand, are designed to match the patient’s anatomy exactly. This eliminates the guesswork during surgery and ensures better outcomes."
Which cases are the right fit for TMJ arthroplasty?
The first step to a personalized approach is patient selection. In a webinar on enhancing TMJ arthroplasty precision with personalized guides, Dr. Thiem emphasized this point and elaborated on the primary indications. These include:
- end-stage TMJ disorders, such as severe arthritis or post-traumatic damage;
- therapy-resistant pain that significantly impairs quality of life;
- and congenital deformities, such as ankylosis or joint malformation.
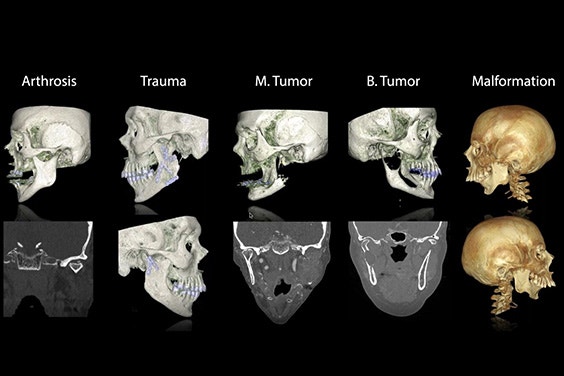
Overview of the different known pathologies for total TMJ replacement and how the cases look when a TMJ prosthesis is used. Image credit: Dr. Daniel Thiem
However, there are also contraindications to keep in mind for this procedure. Dr. Thiem said, "The use of a total TMJ should be avoided with patients who cannot understand the procedure or have unrealistic expectations, like having the same mouth movement they remember from their past." These contraindications are joined by those involving the patient's health, including allergies to the implant material, uncontrolled malignancy, poorly managed systemic diseases, and poor bone quality that would not be conducive to proper implant stabilization.
To illustrate his points, Dr. Thiem shared patient cases, one of which was a patient with severe jaw malformation and restricted mouth opening who regained nearly full functionality post-surgery. “The personalized implants have an excellent fit, and they especially have an excellent fit in complex situations,” said Dr. Thiem.
Balancing function and aesthetics: merging TMJ arthroplasty and orthognathic surgery
In many cases, orthognathic surgery and TMJ arthroplasty are interconnected. Whether the TMJ pathology is the reason behind the orthognathic surgery or vice versa, personalized solutions offer significant value.
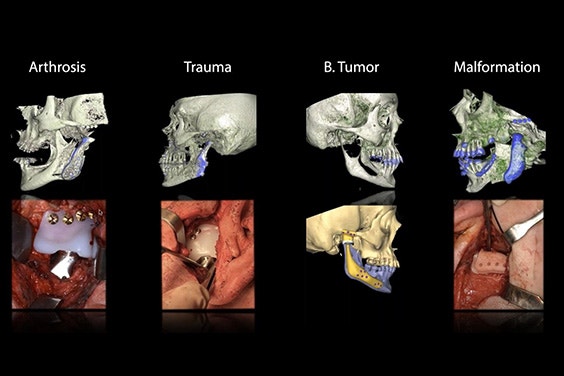
Adding to Dr. Thiem's discussion on pathologies, Dr. Thomas Kofod, Chair of Oral and Maxillofacial Surgery at Rigshospitalet in Denmark, shared his experience combining both procedures.
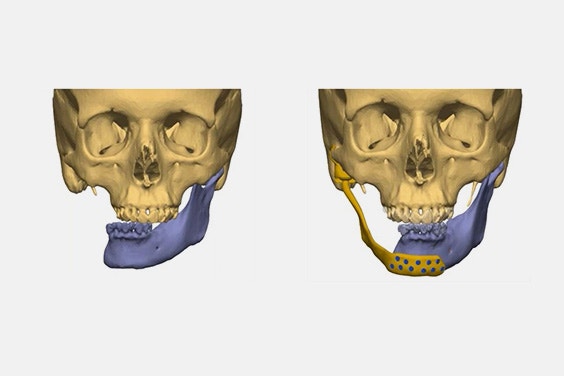
In one case, he treated a patient with a decade-long history of restricted mouth opening and severe osteoarthritis. "Using Materialise’s digital workflow, we planned the procedure with remarkable accuracy, achieving a balanced jaw structure and improved airway function," he says.
"I think there's a great benefit to combined virtual surgical planning for total joints, patient-specific instrumentation, dentofacial deformities, post-traumatic deformities, and reconstructive needs. Personalization leads to an improved fit and, therefore, improved precision."
The preoperative virtual surgical plan and the postoperative result when using a personalized TMJ prosthesis. Image credit: Dr. Kofod
PD Dr. Dr. Rüdiger Zimmerer agreed during a webinar on TMJ solutions for tumor-affected joints and beyond. The Senior Consultant and Deputy Director at University Hospital Tübingen's Department of Oral, Maxillofacial, and Plastic Facial Surgery emphasized the power of personalized implants in addressing both functional and aesthetic concerns. He finds particular value in referencing the preoperative plan during the live procedure.
"One of the best methods is fusing the virtual plan with your operative result while the patient is still under anesthesia. By comparing the two, you check whether you have properly placed the patient-specific implants," shares Dr. Zimmerer. "And if there's a mistake, then you would already see it. The possibility that something will go wrong — if you have done the proper planning and everything works fine — is almost impossible."
In addition to virtual surgical planning, Dr. Zimmerer is impressed by the precision and improved outcomes made possible by combining techniques: "We can show, in many cases, a significant improvement in the maximum mouth opening and a significant reduction in TMJ pain."
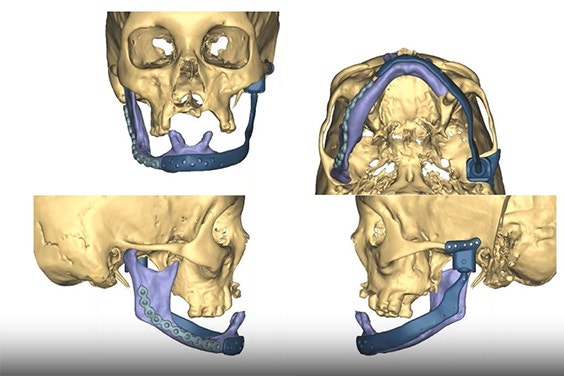
Example of a virtual surgical planning session for a personalized TMJ implant.
Managing TMJ tumors with personalized solutions
TMJ tumors are rare, but personalized solutions also offer value here for complete resection and reconstruction. In the same webinar, Dr. Vladimír Machoň — a Temporomandibular Joint Surgeon affiliated with the Charles University and Faculty Hospital Prague, the Hospital Ceske Budejovice, and private TMJ offices in Prague, Pilsen as well as the founding member of the ESTMJS and a member of the AOCMF — provided insights into the related challenges and reconstruction techniques.
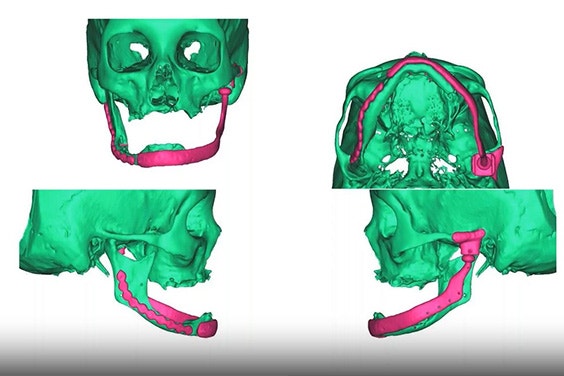
Dr. Machoň explains that, after diagnosing the TMJ tumor with X-ray, MRI, or CT scans, "surgical planning is clearly preferred for both planning treatment of the tumor and reconstruction." He uses a virtual surgical planner to plan the resection line, patient-specific prosthesis, primary reconstruction, and secondary reconstruction.
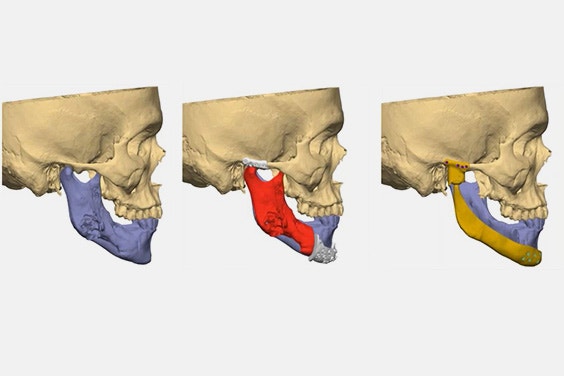
Primary reconstruction plan (left) and secondary reconstruction plan (right): TMJ reconstruction can be performed as primary (immediate) or secondary (deferred) procedures; primary reconstruction involves one operating time with complete tumor removal and a personalized TMJ prosthesis, while secondary reconstruction, often with virtual surgical planning, is done when there’s uncertainty about complete tumor removal, as seen in patients after mandible resection and reconstruction with a personalized TMJ implant.
Dr. Machoň expanded upon his use of virtual surgical planning and personalized implants with takeaways from specific primary and secondary reconstruction cases: "The advantage of personalized prostheses is a shorter operating time. They also respect the anatomical condition of the patient's skeleton, offering superior stability and fixation compared to stock prostheses in some cases." However, he does find value in using the two implant types in tandem for some situations, like when there's not enough time for planning and production of a personalized alternative.
In this field, you always need to consider if radiotherapy is a factor. Dr. Machoň recommends waiting at least 14 weeks after radiotherapy to complete a TMJ replacement surgery, mitigating the risk of implant infection.
Expanding use of personalized solutions
The takeaways from all our webinar guests are clear: personalized solutions are reshaping TMJ arthroplasty. Our TMJ Total Arthroplasty System offers a comprehensive solution, including virtual 3D surgical planning and personalized guides and implants that feature temporal and mandibular components. "The titanium guides are game-changers," said Dr. Thiem. "They offer pinpoint precision, are low profile, and don't require large incisions."
TMJ arthroplasty is no longer just about addressing physical defects — it's about delivering holistic solutions. Surgeons are balancing aesthetics with function and patient outcomes, and the work these pioneers have accomplished with the TMJ Total Arthroplasty System illustrates these advantages clearly.
L-104545-01
Share on:

Biography
PD Dr. Dr. Daniel Thiem

Biography
Dr. Thomas Kofod

Biography
PD Dr. Dr. Rüdiger Zimmerer

Biography
Dr. Vladimír Machoň
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
