INTERVIEW
How Using 3D Printing Has Improved Patient Outcomes at Nemours Children's Hospital
Seamless collaboration between teams across the hospital system, better surgical results and achieving true informed consent with patients. These are just three of the many reasons Nemours Children’s Hospital uses an in-house 3D printing service.
The lab in Orlando, Florida, has grown since it began in 2016. Today it prints 25 to 30 models a month, for a variety of departments across the hospital system. These could include cardiology, orthopaedic, general and plastic surgery, urology, and neurosurgery. The 3D printing team also provides remote support to the system’s sister hospital in Delaware and clinics in Jacksonville and Pensacola.


The 3D printing lab team members Dr. Tushar Chandra, Pushpak Patel, and Dr. Craig Johnson gave us insights into their 3D printing service at Nemours, and developments they hope to see in the future. Part one details the process of setting up their lab, including which software and hardware they use, and part two focuses on the benefits they have seen for their institution and patients.
What was the driver to set up the 3D printing service at Nemours?
It was threefold. First, through conversations with surgical leadership, physicians began making comments on how they wished that they could use 3D printing techniques to see the orientation of the structures on which they were going to operate. This was an initial spark to start funding for the project.
Second, educationally with our own patients, we knew it would improve communication and understanding. Before 3D-printed models, we used commercially produced ones of anatomic regions to explain the disease processes and the risks of certain procedures. However, we would sometimes work with the rare diseases that do not have commercially produced models available. We knew in other rare specialties that this would also be a significant benefit for the important decisions both clinicians and families have to make.
Third, we had a vision of personalized medicine towards simulation so that the most complex patients could have their unique disease and anatomy rehearsed before the first incision was made. Seeing the anatomy in 2D on a CT or MRI was an advancement, but for those who operate in 3D we felt this would be the best and would lead to better outcomes, decreased complications, decreased operating room time, and decreased cost.


Why do you believe radiology is well-positioned to support 3D printing?
We believe that radiology is the most suitable department to support a 3D printing service. This is primarily because radiology is an integral and a central part of the diagnostic framework of hospitals and health care systems throughout the world. Imaging studies and protocols are formed, as well as interpreted, by the radiology department. And radiologists and radiology technicians are specially trained to acquire optimal images to answer relevant clinical questions. These questions go a long way in making complex decisions by clinicians and surgeons.
What is the structure of your team?
Our team consists of our program director, Dr. Craig Johnson, along with our co-director, Dr. Tushar Chandra. Pushpak Patel is the lead of the 3D printing service, and works with our CT and MRI groups to make sure we get the right imaging for the models. The team also includes two technicians who perform the segmentation and modeling, and we foster a collaboration with University of Central Florida (UCF) who provide additional resources for specific types of modeling and printing.
What exactly is the lab doing today?
When we first started using these new technologies, the big concern was that sometimes your ideas were ahead of what the software could do. So I remember in the beginning we had a lot of ideas, but the computer said no. And now it’s fantastic that the only limitation is your individual know-how.
Today, before every 3D planning we meet the surgeon pre-operatively to discuss the position of the implants or the design of the guides. Once approved, we visualize the plan for the patient and surgeon and put the data in the patient file. When asked, we join the surgeon and patient in the clinic to explain the technical side of the intervention.
Which hardware and materials are you using?
We use many technologies including SLA, DLP, FDM, and Polyjet. The decision-making process for what printer and material to use depends on the surgeon’s needs, requirement of the model, complexity of the anatomy, coverage required, and timeline. All of these aspects come into play to help our in-house experts make a decision.
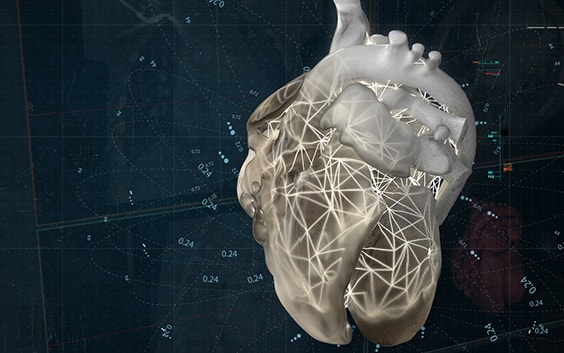
How has Materialise Mimics software either enabled your work or enhanced your work?
Accuracy of the model is driven by the software. If you have good software, your models will have a better quality. With software such as Materialise Mimics, it helps to ensure that we are building accurate models for our surgeons and patients. Thanks to Mimics inPrint, we can verify the accuracy of our models by superimposing the 3D-print-ready file onto the CT or MRI data. This enables us to ensure sub-millimeter accuracy of our models. The usability of software is also important. With Mimics inPrint, the software is very well organized with five simple steps. It makes the segmentation and modeling efficient by working in a single software interface and workflow.
Additionally, the cloud based Mimics Viewer allows us to collaborate on cases with our surgeons working in remote facilities. The surgeon can review, provide input, and confirm accuracy of a model prior to proceeding with the printing process. It enables us to easily work with teams that are based remotely, such as the team at our campus in Delaware, a thousand miles away. We can send them a link of the cloud viewer, they can open it up on their computer, tell us what they see, and we can go from there.
Mimics is available on any hardware in our medical center, and because of that, we can pick up the work from any computer in the hospital. We have two offices, one at the lab and one at the hospital, and we go back and forth between the two. We can open Mimics from anywhere and start working from where we left off on any computer.
More broadly, Materialise’s software is very important for 3D printing in healthcare because hospitals around the world are working on the same platform. We think having one software that all of us are using is a big way to make sure that we speak the same lingo. We can share cases and we can learn from each other's techniques to further advance patient care across the globe.
What are the main benefits of having a printing service at the point-of-care?
3D printing is a novel tool that is transforming healthcare in a very unique way: we are increasingly entering the area of personalized medicine, in which we have a true personalized 3D model. And it's something that we have never seen before.
In the medical field, this directly impacts the experience a patient and their family has with healthcare systems. If you give them a 3D model that they can see with their eyes, they have a much better understanding of what is going on. And they don't have to rely on modalities like ultrasound, CT, or MRI, of which they do not have a fundamental knowledge of understanding.
Unanimously, all the surgeons we talk to really love these models, and they prefer using them – especially if they are working on a complex case. These models are very beneficial because the surgeon can look at the models as they would encounter the patient’s anatomy when they are in surgery.
This is something that has never happened before: surgeons can plan a personalized approach before going into the operating room. Many studies have shown that this technique has resulted in decreased operating room time, decreased surgical blood loss, and decreased surgical morbidity. To them, these models are a whole lot different from looking at cross-sectional studies and simply going by whatever the radiologist tells them.
Getting a better understanding of what the actual size would be within the patient's body is useful to them, especially if they're dealing with small sectors and microsurgeries. This is an enormous benefit for us.
How is 3D printing adding value for Nemours as an institution?
Apart from the clinical care itself, we think 3D printing has possibilities for education and research. We are already using it as an important tool for educating medical students, residents, and colleagues, such as physicians and surgeons. There is no substitute for looking at an organ or a set of organs in a 3D format in front of your eyes, which is actually identical to how it exists within the body. If we take a model to a lecture, we can clearly see that the understanding of anatomy, which can be complex, is much better. Plus, the confidence that trainees have in really understanding that part is greatly improved.
Nemours has always fostered innovation and research as a way to do whatever is the best for our patients. We strongly believe that 3D printing is the way to go for the future: there is nothing more innovative and more novel than 3D printing within the diagnostic team. It truly increases the satisfaction level and the understanding that patients have about complex cases and makes decision-making easier for families.
Could you please tell us about a specific case in which you used 3D printing?
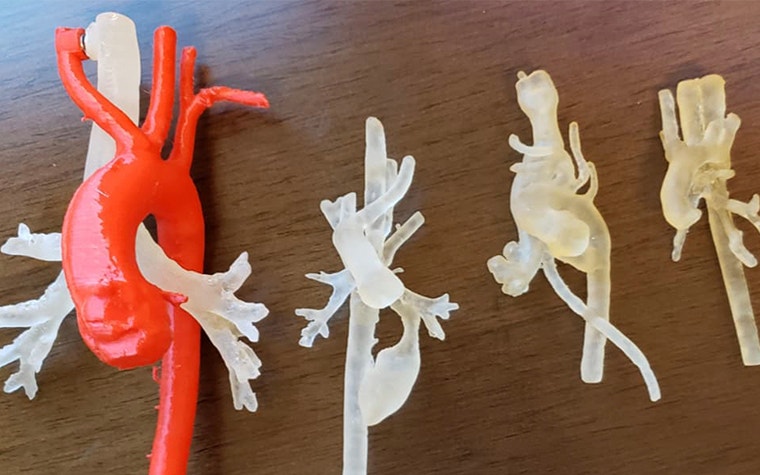
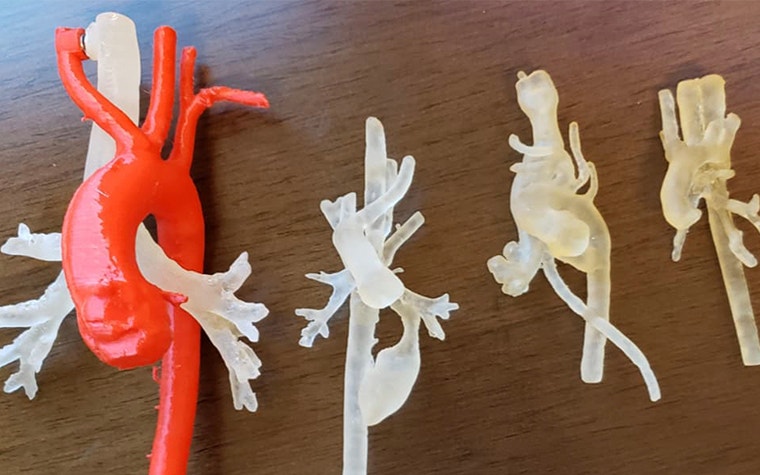
We actually have two we would like to share. The first is with a case where a surgeon was planning to remove a five-year-old child’s entire left kidney because of a tumor. With the assistance of a model, she was able to re-examine the surgical approach, and even do the surgery on the model before going into the operating room. She was able to practice on the model, by cutting the tumor out, and see the blood vessels and all the urinary tract systems that would be involved. She could also take this model and show the family members so they knew exactly what was going on with the child.
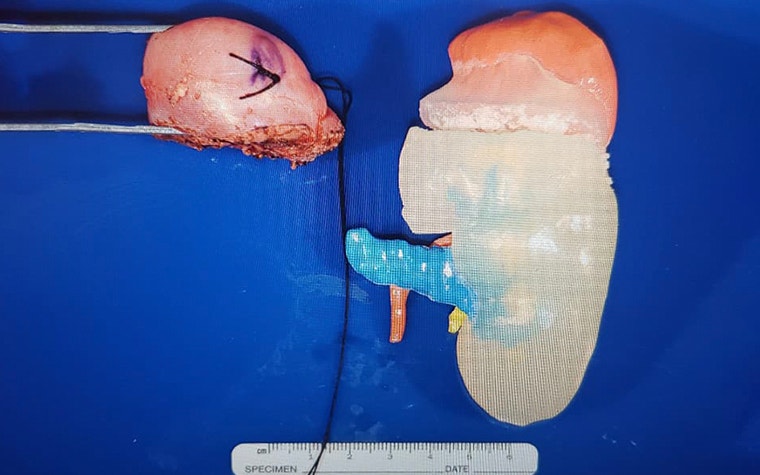
Because of the model, we know she was able to save 75% of the kidney instead of removing the entire organ.
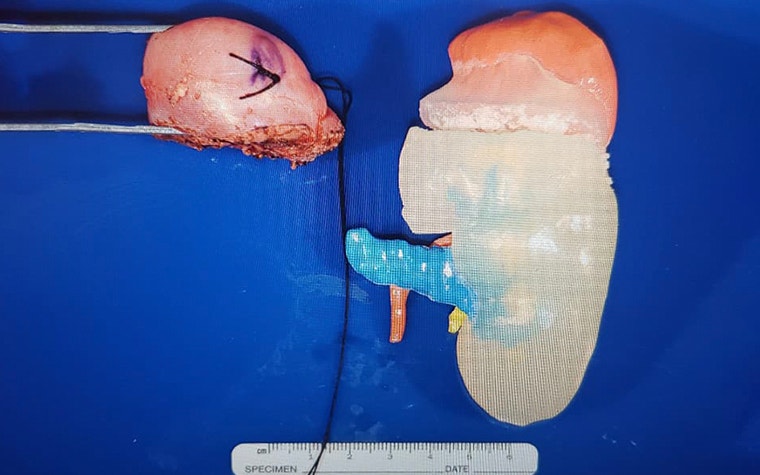
There is another case we’d like to share of a child who had a large malignant tumor near their shoulder. It was coming from the scapula and was very close to the vessels in the region, making it a complex case. We had a team of specialists discuss this case in a conference and we decided to make a 3D-printed model. The idea was to show the model to the family because the surgeon wanted to have the opinion of the patient's family to decide whether to opt for surgery or chemotherapy. This is a difficult decision for a family to make, so we wanted to ensure they understood the pros and cons. In the end, the family was able to make a better-informed decision with the 3D model in hand.
They decided to opt for chemotherapy, and after the treatment we printed another model. The change was remarkable: it was amazing to see how much the tumor shrank. When this model was again taken to the clinical visit, the patient and their family could compare side by side the pre-treatment versus post-treatment tumor. It was incredible: the tumor was a big ball to begin with, and it went down to the size of a peanut.
You could not achieve the same interaction with any MRI or CT that you show to a family. We think that is where 3D printing really makes a difference. They could see that the chemotherapy was really working, and doing what we wanted. The understanding was much better than what you would have achieved with any diagnostic scan.


From your perspectives, what do you think are the most important needs in order to support the continued growth of this technology in medicine?
We think that we are still in an infant phase as far as 3D printing goes in the medical field. But there are many potential things that must happen to sustain this growth. There is nothing more important than spreading knowledge and awareness about the role 3D printing has to play in transforming healthcare. So all of us and our team try to spread information amongst our peers, other fellows, and surgeons on a case-to-case basis, and overall, such as how 3D printing can impact decision-making and enhance the patient experience.
Other than that, from an infrastructure point, we think it's important for the technology to sustain itself. More specifically, we think reimbursement and insurance are big factors in that. We feel like once that happens, it will be the thing that really sets everything in place.
Up to now, we have been using money that has come from various projects, or there have been several benefactors who have donated for this specific technique. We think for anything to sustain itself, support has to come from within. So, that is the second-most important need.
The third thing that has to happen is that we have to grow in terms of research and technique. 3D printing has grown a lot, but we should continue to research and find new clinical applications. Printers that work faster. Printers that can deal with complex anatomy. All the research that has been happening must go on so we can educate people, access the financials, and continue to grow the field. Then there's no reason why this would not sustain and grow in the future.
L-100664
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.