EXPERT INSIGHT
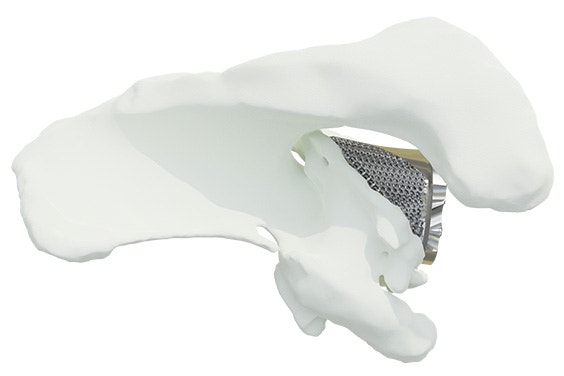
Complex Glenoid Deficiencies: Indications for 3D-Printed, Patient-Specific Implants

In recent years, there has been a growing trend toward utilizing patient-specific implants to manage complex glenoid deficiencies. According to the literature, patient-specific implants offer a promising solution for treating severe glenoid defects.1,2 For instance, a study by Debeer et al. concluded that adequate pain relief, reasonable functionality, and good patient satisfaction can be obtained for difficult cases. But what defines a ‘difficult case’? Where do the boundaries of bone grafting and augmented baseplates lie? And when should a personalized implant be considered?
When do surgeons turn to personalized solutions?
In the evolving landscape of orthopaedic surgery, utilizing personalized implants remains a subject of debate. So, we performed a retrospective analysis to gain insights into when surgeons opt for personalized glenoid baseplates.
Based on this analysis, primary shoulder arthroplasties constitute 38% of cases involving significant glenoid bone loss, while hemi-revisions account for 16%. Total shoulder revisions make up the remaining 46%.
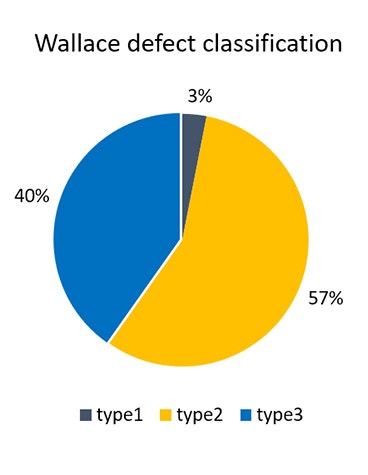
These cases primarily involve patients presenting with Wallace type 2 or 3 defects, characterized by erosion beyond the lateral base of the coracoid or extending further than the medial spinoglenoid notch.3,4
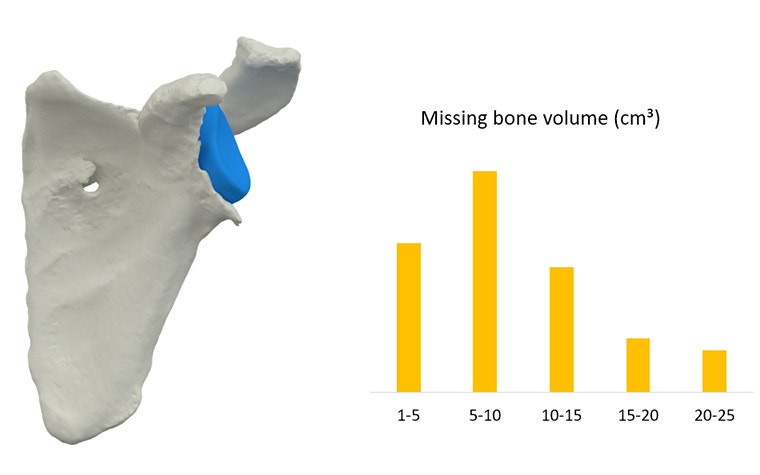
Comparison with a statistical shape model5,6 shows that the majority of these patients experience glenoid vault loss ranging between 5 and 10 cm³ (0.3 – 0.6 in³), with some cases extending up to 25 cm³ (1.53 in³).
In summary, this retrospective analysis reveals that surgeons choose personalized baseplates for both primary and revision shoulder arthroplasties involving significant bone loss.
With these insights in mind, we proceeded to explore four specific case types, outlining the challenges associated with each of them.
Challenge 1: Severe medialization of the glenoid face
Shoulders with a severely medialized glenoid face present a unique challenge, as a correct implant position and orientation are crucial for optimal patient outcomes7,8. However, this is not always straightforward to achieve when facing an extremely eroded glenoid vault. Structural bone grafts can fill substantial voids and restore lateralization, but large grafts may lead to early loosening and implant failure if fixation within the native bone is insufficient.9


Challenge 2: Excessive glenoid version
Glenoid defects with excessive version can also present significant difficulties.10 Securing a stable fit with a structural bone graft can be difficult, as the graft needs to fit precisely and the oblique glenoid surface can cause the graft to slide off easily. Alternatively, reaming the surface to decrease the glenoid version is an option, but it requires removing extra subchondral bone — a risky proposition when glenoid bone stock is already limited.
Challenge 3: Central cavity in the glenoid bone
After a failed (reverse) total shoulder replacement, the situation can become even more complex. Especially when the failed implant contained a central peg or post. When a central area is severely eroded, limited bone remains for screw placement, increasingly complicating subsequent interventions.


Challenge 4: Completely eroded glenoid vault
Finally, when facing a completely eroded glenoid vault, it is almost impossible to obtain sufficient implant-to-bone support when using a standard baseplate.
Moreover, the limited remaining surface makes it hard to find a stable fit for such baseplates, and placing screws becomes challenging due to the restricted bone volume available for fixation.


Indications and contraindications for personalized glenoid baseplates
The four types of glenoid defects discussed in the previous sections highlight indications for utilizing personalized glenoid baseplates, as these implants offer tailored solutions to address the challenges encountered.
In cases with severe medialization of the glenoid face or excessive glenoid version, personalized glenoid baseplates can restore the lateralization and orientation of the glenoid since these implants can be meticulously shaped to fill the eroded glenoid vault using the patient’s CT scans. 1,2
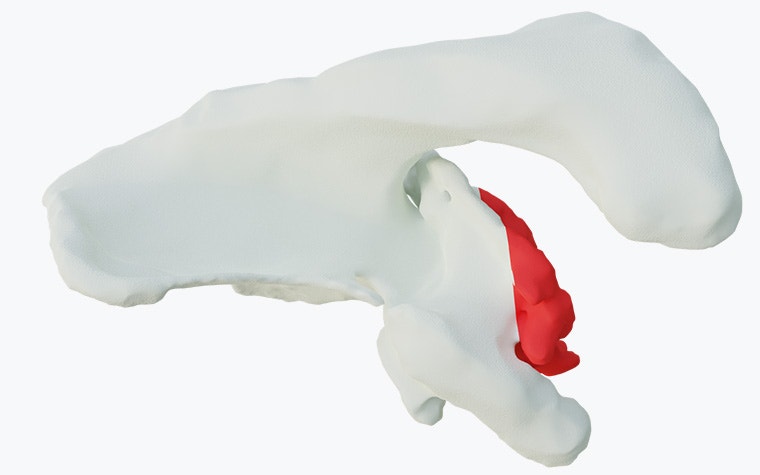
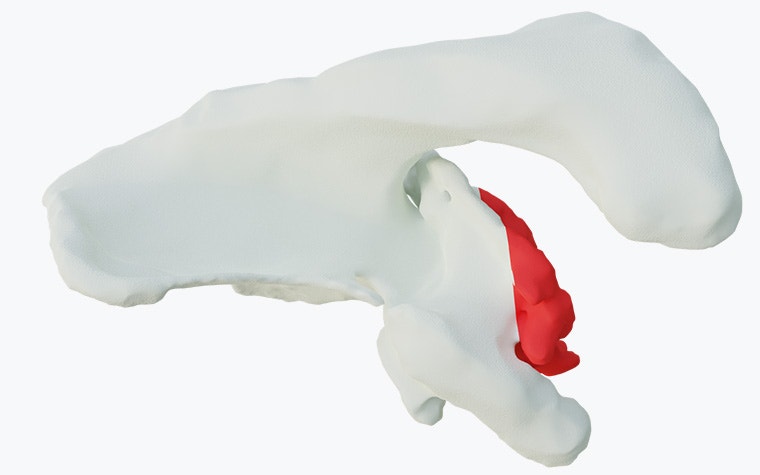
For cases with a central cavity in the glenoid bone or a completely eroded glenoid vault, personalized implants can offer secure implant fixation due to the ability to plan patient-specific screw trajectories. Additionally, 3D-printed guides can aid in precise implant positioning and screw placement, ensuring stability and proper alignment.
Contraindications for personalized implants are active infections, sepsis, and axillary nerve deficiency11 — similar to those for standard implant components.

Key takeaways: the advantages of personalization
Our retrospective analysis of shoulders with significant glenoid bone loss highlights key indications for personalized implants, observed in both primary and revision shoulder arthroplasties.
These indications can be categorized into four groups:
- Severe medialization of the glenoid face
- Excessive glenoid version
- A central cavity in the glenoid bone
- A completely eroded glenoid vault
Personalized implants offer tailored solutions designed to overcome challenges in shoulder arthroplasty procedures associated with these indications. Understanding and recognizing these indications is essential for informed decision-making in surgical interventions.
L-104037-01
3 Based on a retrospective analysis conducted at Materialise
7 Strauss et al. The glenoid in shoulder arthroplasty, J Shoulder Elbow Surg, 2009
11 Instructions for Use of the Materialise Glenius Glenoid Reconstruction System
Glenius is not yet commercially available in the US and Canada.
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
