CUSTOMER STORY
Interactive 3D Planning for Congenital Heart Disease: Improving Outcomes at Hannover Medical School

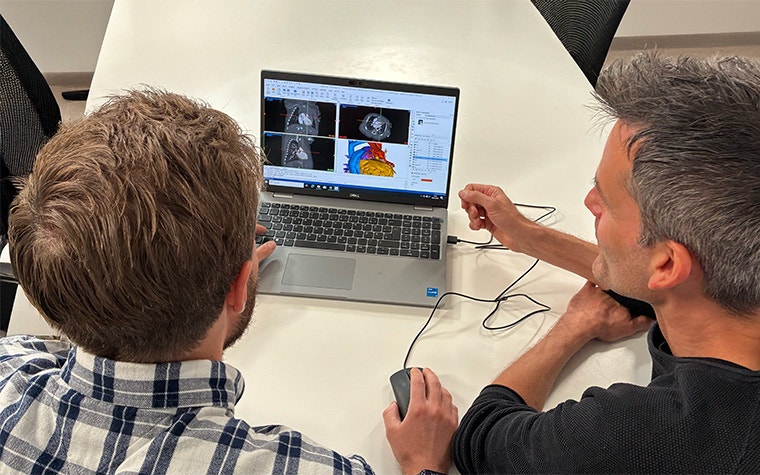
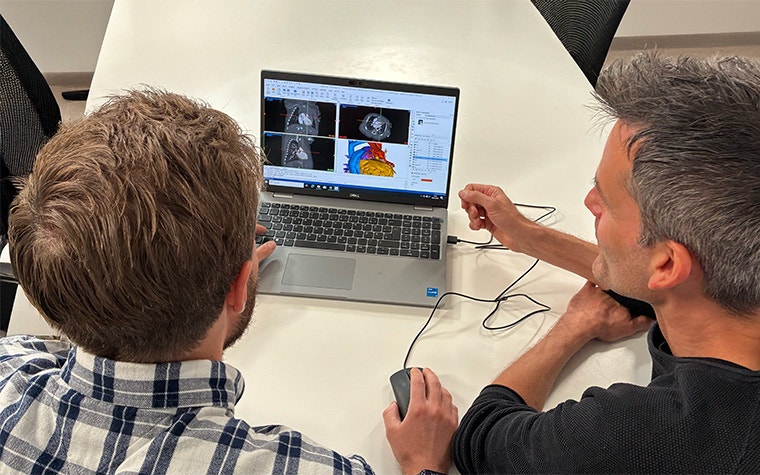
In the pediatric cardiology wing of Hannover Medical School, a team huddles around a screen. Surgeons, cardiologists, radiologists, and engineers are deep in discussion — not over 2D slices, but around a 3D model of a child’s heart.
Dr. Christoph Happel, a Senior Physician and Head of the Cardiac Catheterization Laboratory, leads the discussion, posing questions like “What if we patch here?” and “Will we clear the coronary?”
The 3D virtual model belongs to a child who will be in the operating room within days. And these conversations amongst the heart team, plus the clarity from interactive 3D planning, are critical to the outcome of the procedure.
“Understanding is the first thing you need to provide proper treatment to your patient. Interactive 3D models give us that clarity instantly.”
— Dr. Christoph Happel
The biggest insights into the smallest hearts
Treating congenital heart disease is like solving a 3D puzzle. But for too long, clinicians have tried to solve it with 2D CT or MRI slices and diagrams scribbled on a piece of paper. Dr. Happel remembers the frustration well: “We would spend 30 minutes just convincing everyone where specific vessels are located,” he says.
They had explored better ways to analyze CT and MRI data sets, seeking a tool that translates data into 3D-segmented models capable of accurately representing complex cardiac anatomies. To give the best care possible, they needed deeper insights into medical issues. And the window of time between imaging and surgery is short — often just days.
If these insights were wrapped into an interactive 3D model, the entire heart team could start treatment discussions with a shared foundational understanding, supporting better preparation and clinical decisions.
The search for the right tool ultimately led them to Materialise Mimics — software that converts MRI and CT scans into precise, interactive 3D models. In just 30 – 45 minutes, technicians segment each structure — atria, ventricles, great vessels, surgical grafts from prior operations — for a finished model that can be color coded, rotated on any laptop, viewed in extended reality, or 3D printed for hands-on planning.
The impact was immediately evident: “Now, the anatomy speaks for itself in seconds. It shows in a very clear, intuitive way what the pathology in a patient looks like.”


Interactive 3D planning drives efficient preparation and surgical precision
What once took the team hours of manual effort, they can now achieve in under an hour. They've seamlessly integrated 3D modeling into their workflow and use it regularly, handling an impressive 7 to 10 cases per week. For patients with complicated anatomies or who have had previous operations or re-thoracotomies, the insights 3D visualization brings are especially valuable. They help the team prepare for complex cases faster and align with the hospital’s goal of improving patient outcomes.
In each case, the Hannover Medical School team sees the same advantages:
- Better preparation for complex cases. Multidisciplinary teams don't require the extra alignment time before they make important decisions. Interactive 3D planning aligns the entire heart team with the same anatomical understanding. Instead of debating orientation, they can focus on refining the surgical approach.
- Enhanced interventional and surgical precision. With virtual planning, the surgeons and interventionalists can practice the procedure in a risk-free environment. The team gains more confidence in their stent placement or patch sizing before entering the procedure. In fact, 71% of clinicians in a 2018 study reported improved management of postoperative problems in congenital heart disease surgeries with interactive 3D models.
- Simplifying complex reoperations. Children with prior surgeries often present scar tissue and unusual vessel paths. Interactive models let the team expand surgical options for complex cases and map safer incision sites to reduce operative time and bleeding.
- Family trust. Anticipating a young loved one's heart surgery undoubtedly brings great stress. It doesn't help that procedures like these are difficult for the families to understand. Now, the team explains the treatment to the parent alongside a 3D model of their child's unique heart, not an abstract diagram. Trust grows when they see exactly what's wrong and the proposed treatment.
“I love to have a clear understanding of what the anatomy looks like and to share this knowledge with other people," explains Dr. Happel. "A 3D model is so much more intuitive than 2D slices. Understanding is the first thing you need to provide proper treatment to your patient. Interactive 3D models give us that clarity instantly.”
“We’re at the beginning of discovering the real value of 3D and simulation in clinical contexts.”
— Dr. Christoph Happel
Beyond patient cases, this technology also plays a significant role in preparing the heart team of tomorrow. The Hannover Medical School team collaborates with LMU Munich to offer a course for trainees in pediatric cardiology.
3D-printed models are their tool of choice for educational purposes: "The young medical doctors love the printed models because you can literally do everything you'd do in a patient, but you don't have to worry about something going wrong. It's perfect."
Significant wins inspire community support
Dr. Happel’s lab pioneers life-changing advancements, but the financial reality remains challenging. There is still no dedicated reimbursement code for 3D planning in most European health systems.
Luckily, PSD Bank Hannover stepped in. Recognizing Dr. Happel's impact, the community bank rallied donors for a special fundraising drive to finance the right tools and staff training, fast-tracking the lab’s vision to model every complex CHD case that arrives in Hannover.
Happel and his team are grateful for the partnership: “Without PSD Bank’s initiative, many children would still be waiting for technology we already know can help them.”
“That’s our biggest hurdle,” Happel admits. “The value to the child is undeniable, but these programs survive on crumbs and donations.”
What's next for 3D planning?
The heart team at Hannover Medical School has taken significant strides, but they're not done innovating.
Dr. Happel would like to take virtual surgical planning a step further by including other modalities in the model, such as the valve structures obtained from echocardiographic data.
He also has hopes in simulation developments: "By simulating the planned measures on the model to visualize the results in advance, I hope we'll be able to identify the best alternative for the patient even faster."
For Dr. Happel, this is just the start. He recommends clinicians in other medical specialities consider the impact 3D technology could have on their fields: "Whenever you work with patient anatomy, it’s worthwhile to visualize it as a digital twin or 3D model, either printed or virtual. We’re at the beginning of discovering the real value of 3D and simulation in clinical contexts."
L-104673-01
Materialise medical device software may not be available in all markets because product availability is subject to the regulatory and/or medical practices in individual markets. In countries where no regulatory registration is obtained of Mimics and/or 3-matic Medical, a research version is available. Please contact your Materialise representative if you have questions about the availability of Materialise medical device software in your area.
Share on:

Biography
Dr. med. Christoph M. Happel, PhD
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
