CASE STUDY
Precision in Pediatrics: Skull Reconstruction with Virtual Planning and Augmented Reality
In Córdoba, Spain, children who once faced daunting medical challenges can now enjoy a healthier start to life thanks to pioneering surgeons at Reina Sofía University Hospital. For the pediatric cranio-maxillofacial (CMF) department, every millimeter matters. That's why the surgical team has a mission to improve precision with virtual 3D planning, 3D printing, personalized CMF guides, and augmented reality (AR).

Industry
Cranio-maxillofacial surgery
Key solutions
- Virtual 3D surgical planning
- Augmented reality
- 3D-printed anatomical models and personalized CMF guides
The impact
- Enhanced surgical precision
- Reduced risk in the OR
- Improved functional and aesthetic outcomes
The challenge
Complex pediatric cranial reconstruction
Cranial reconstruction is an intricate procedure. When performed on a small child, it's even more so. The challenge is in addressing the delicate nature of the patients with the precision necessary for neurosurgery.
Congenital malformities such as scaphocephaly and trigonocephaly require finely detailed work, both in the preparation and surgical execution, to achieve the functional and aesthetic outcomes these young patients deserve.
At Reina Sofía University Hospital, surgeons recently faced this particular challenge in the case of a nearly two-year-old patient with scaphocephaly. To support their surgical plan, the team collaborated with one of our clinical engineers to define osteotomies, reposition in 3D, and design personalized cutting guides and position guides. Based on the virtual planning, anatomical models were then 3D printed to assist in preoperative preparation.
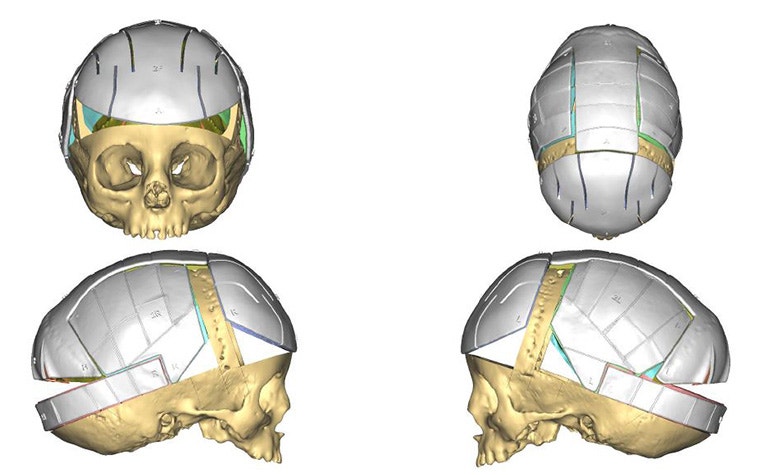
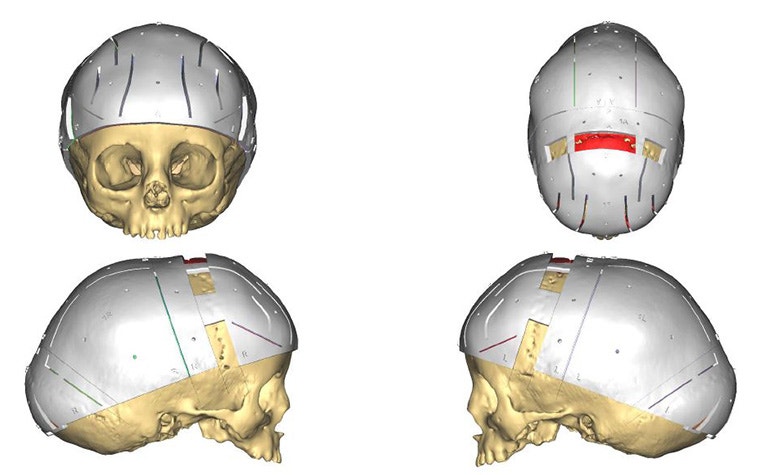
3D-printed and positioning and cutting guides support the accurate transfer of the surgical plan to the OR.
The solution
Virtual 3D planning with an AR integration
The pediatric neurosurgery team, led by Dr. Juana Vidal, used virtual surgical 3D planning, 3D printing, and AR to enter the OR fully prepared.
To begin the surgical planning process, they incorporated medical images from MRI and CT scans into virtual 3D planning software. The virtual 3D model they created with this data offers various paths forward: planning within the software itself, 3D printing anatomical models, and AR visualization.
The 3D-printed replica provided them with a visualization of the anatomy they can physically hold in their hands and practice with.
AR, on the other hand, let them rehearse the procedure in a digital setting. "Virtual planning allows us to perform the surgery before the actual surgery," says Dr. Vidal. "With augmented reality glasses, we can visualize the final outcome we aim to achieve and plan each cut and remodeling step with precision."
The use of AR didn't stop at the OR door. The surgeons also used technology during the surgery itself. AR provided a real-time comparison of the actual bone cuts with the preoperative plan, so the surgeon could ensure the alignment was as precise as possible and make adjustments when necessary. They could visualize the final outcome before making a single incision.
For more support in the OR, the team used personalized CMF cutting guides and position guides to support the accurate transfer of the surgical plan. These 3D-printed guides — produced in polyamide or titanium — help ensure that bone cuts are made as planned, contributing to greater predictability and safety in surgeries where accuracy is critical.


The result
Efficiency, precision, and reduced risk
This combination of techniques provided ample advantages to both the team and the patient: "We can plan every step of the surgical intervention before performing it, improving both aesthetic and functional outcomes while reducing surgical times and associated risks."
They meticulously calculated and planned every detail of the surgical approach, from volumes to incision points. And having such a detailed plan made a significant difference during the surgery. "Thanks to preoperative planning, operating room time is significantly reduced, which decreases the need for blood transfusions and enhances patient safety," says Neurosurgeon Dr. Marta Guzmán. "Moreover, aesthetic outcomes are more and more predictable and precise, increasing satisfaction for both families and the medical team."
For this particular patient, the results have been very positive. The team achieved the planned volume and an excellent aesthetic and functional outcome in the shortest time possible. Now, the patient is in very good condition, with no complications from the surgery and good psychomotor development.
As this technology continues to evolve, surgeons will have an even greater level of confidence and control in their most complex cases. According to Dr. Juan Solivera, Head of the Neurosurgery Department, "The combination of virtual planning and AR in surgery represents a major step forward toward more precise, safer, and patient-centered medicine, which is particularly important for pediatric patients with complex conditions."
Images provided by Reina Sofía University Hospital
L-104704-01
Materialise medical device software may not be available in all markets because product availability is subject to the regulatory and/ or medical practices in individual markets. Please contact your Materialise representative if you have questions about the availability of Materialise medical device software in your area.
Featured products and services
Share on:
