CASE STUDY
A 3D Templating Study on Restoring Hip Biomechanics with Cemented Femoral Hip Implants
This case was presented by Prof. Thierry Scheerlinck and Elien de Winter, MD, from the Department of Orthopedics and Traumatology, University Hospital Brussels, Belgium.
Determining the appropriate choice and size of an implant is crucial for relieving pain and restoring mobility in patients requiring total hip replacements. Prof. Thierry Scheerlink and his team wanted to find an efficient way to assess the suitability of two cemented femoral implant systems in a population of 30 patients.

Industry
Healthcare
Key solutions
Materialise Mimics
The impact
Easy scaling of work
Automation of repetitive tasks
The challenge
Compare performance of two cemented femoral implant systems
Total hip replacement is widely considered a very successful surgery to relieve pain and restore mobility to patients. Since the shape of every patient's femur is different, the femoral offset, anteversion angle, and length can vary widely between patients. Therefore, to achieve good functional results, an accurate restoration of hip biomechanics with appropriate implant and sizing options is essential.
Professor Scheerlinck and his coworkers at the University Hospital of Brussels wanted to know whether two different cemented femoral implant systems would be able to restore hip biomechanics (both anatomic and 5 mm medialized rotation centers) in 30 patients.
The solution
Virtual implantations using Mimics' Scripting module
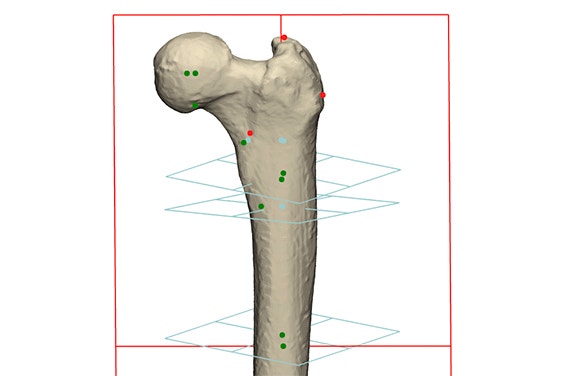
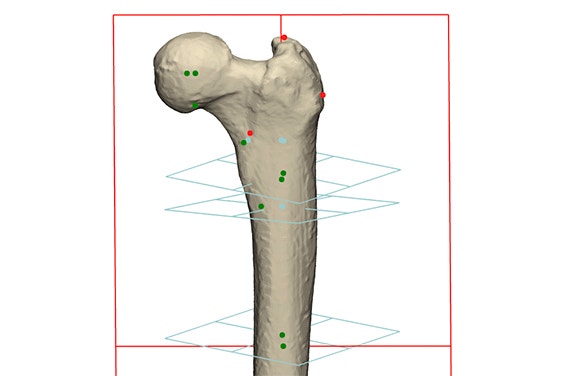
Thirty femurs were segmented, and their hip rotation center, proximal femoral axis, and femoral length were determined (Figure 1). The implants, listed in Table 1, were landmarked and the implants were automatically sized and aligned along the proximal femoral axis to restore an anatomical and 5 mm medialized hip rotation center.
Exeter type (CPT — Zimmer Biomet)
- Sizing options: 18
- Offset options: 5
- Femurs: 30
- Centers of rotation to restore: 2
Kerboul type (Centris — Mathys)
- Sizing options: 12
- Offset options: 4
- Femurs: 30
- Centers of rotation to restore: 2
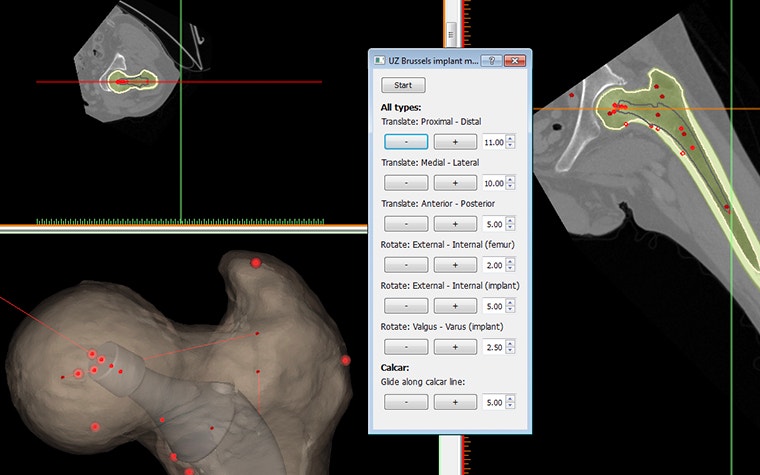
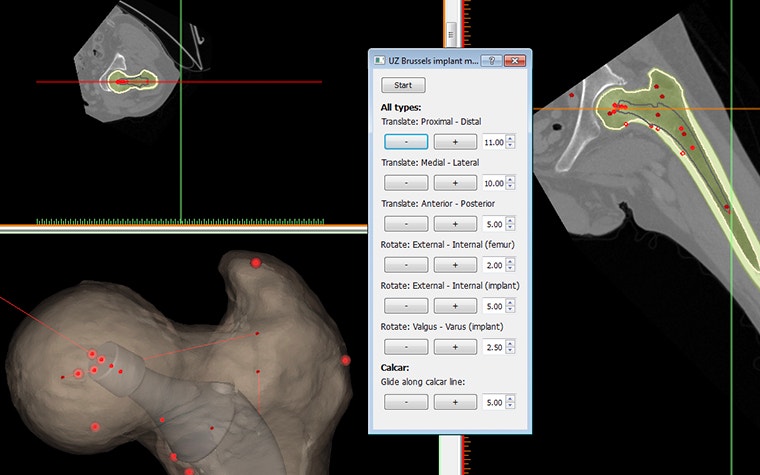
In total, the script took about 10 seconds to generate each stem/femur combination (Figure 2), which would have taken about 30 minutes per combination if performed manually.
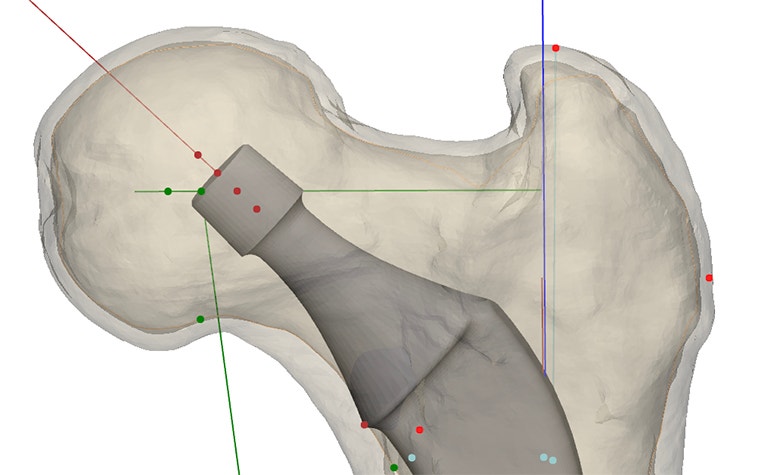
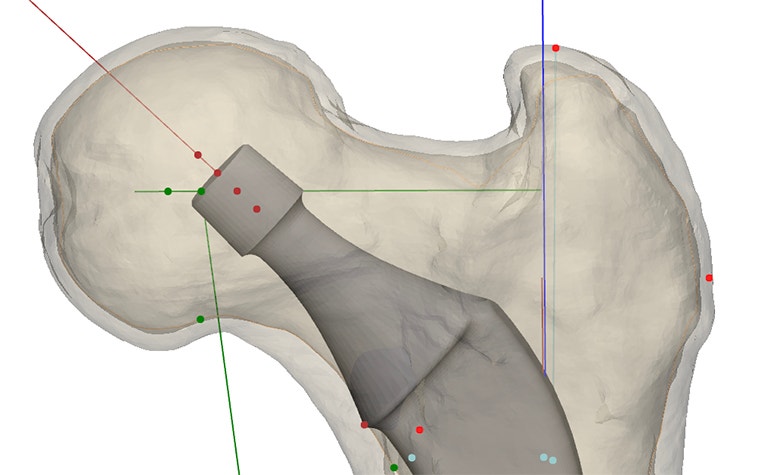
The proposed stem size and position could be manually fine-tuned by the surgeon through a custom user interface (Figure 3). Python allows the user to create user-friendly interfaces and they can be made to interact with Mimics Core and 3-matic.
The Scripting module in the Mimics offers several advantages for studies like this, including:
- scaling of work from one or two patients to dozens or even hundreds of patients
- avoidance of repetitive work and focus on more important tasks
- more consistency between Mimics users
- more user-friendliness and consistency through Python's support for custom user interfaces that interact with Mimics Core and 3-matic
- the Python programming language being relatively easy to learn, with a wealth of knowledge available on the internet
- scripting tutorials that are included in the module, giving a head start on scripting workflows
The result
Superior performance of one system for anatomic and medialized rotation centers
Stems 1 and 2 allowed an accurate restoration of the anatomic hip rotation center (mean distance stem rotation center to anatomic rotation center, Stem 1: 0.97±0.88 mm, Stem 2: 1.66±1.59 mm). Stem 1 allowed the restoration of the rotation center to within 5 mm of the anatomical rotation center in all 30 cases (max. 4.31 mm), whereas stem 2 achieved this in only 28/30 hips (max. 6.72 mm).
Aiming for a 5 mm medialized rotation center was more difficult to achieve with both stems (mean distance stem rotation center to anatomic rotation center, Stem 1: 1.38±1.63 mm, Stem 2: 3.61±2.73 mm). Stem 1 allowed the restoration of the rotation center within 5 mm of the medialized rotation center in 29/30 cases (max. 8.09 mm), whereas Stem 2 achieved this in only 25/30 cases (max. 11.15 mm).
Professor Scheerlinck and his coworkers concluded that although both stem systems allowed the restoration of hip biomechanics accurately in most cases, Stem 1 was superior to Stem 2 for achieving both anatomic and medialized rotation centers. This could be explained by the wider range of implant sizes available in Stem 1 versus Stem 2 (18 versus 12) and that Stem 1 was a so-called 'undersized stem,' offering more freedom to the correct version.
They also found that both stems had difficulties achieving a medialized center of rotation. In some cases, differences between aimed and planned rotation centers were close to 1 cm, which might negatively impact the clinical outcome.
Therefore, they recommend that to avoid suboptimal reconstructions with the available implants, templating should be considered mandatory – especially when aiming for a medialized reconstruction.
L-102657-01
Share on:
