CUSTOMER STORY
How Professor Van Mieghem Makes Calculated Decisions for TMVR Using 3D Planning
When it comes to TMVR procedures, the wrong size implant can lead to severe complications or even prove fatal. As TMVR candidates have high operative risk, their cases are often complex. 3D planning helps mitigate the risk by providing clarity and accurate measurements, allowing clinicians to perform confidently.
We talked to Professor Nicolas Van Mieghem and Dr. Joris Ooms of the Department of Interventional Cardiology, Thoraxcenter, Erasmus University Medical Center located in Rotterdam, The Netherlands, about their use of the Mimics Enlight software for a transcatheter mitral valve replacement (TMVR). The team prepared for the TMVR by first planning the conventional 2D way and then used 3D planning for comparison.
“We believe that 3D planning is now mandatory for TMVR cases. ”
— Prof. Nicolas Van Mieghem, Interventional Cardiology, Erasmus University Medical Center
The patient was a 65-year-old woman, which is relatively young for this type of procedure, but she was morbidly obese, had suffered several strokes, and had many illnesses including hypertension, diabetes, and gout. On top of that, she had mitral valve stenosis, a narrowing of the opening in her mitral valve — based on severe mitral annular calcification. Due to her obesity and diabetes, she was turned down as a candidate for surgery by the center’s heart surgeons.
So, there was no other option than to explore a catheter-based treatment. For most patients who have structural heart intervention, clinicians rely on transthoracic and transesophageal echocardiography and CT scanning. However, the team also wanted to use the most advanced tools they could, which is why they turned to 3D planning for the TMVR.
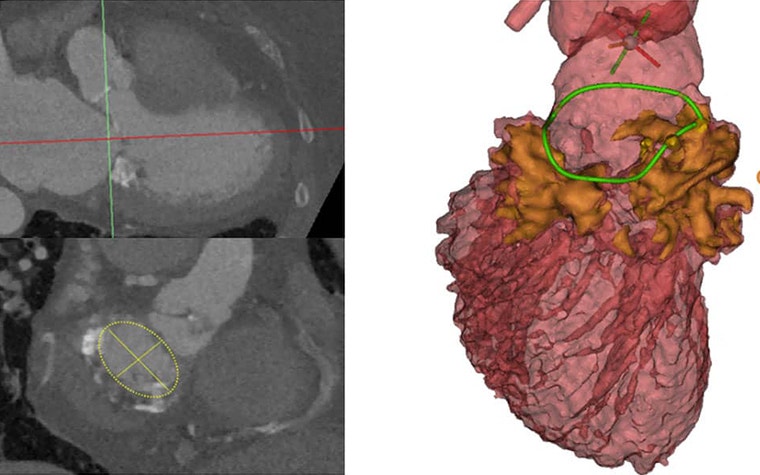
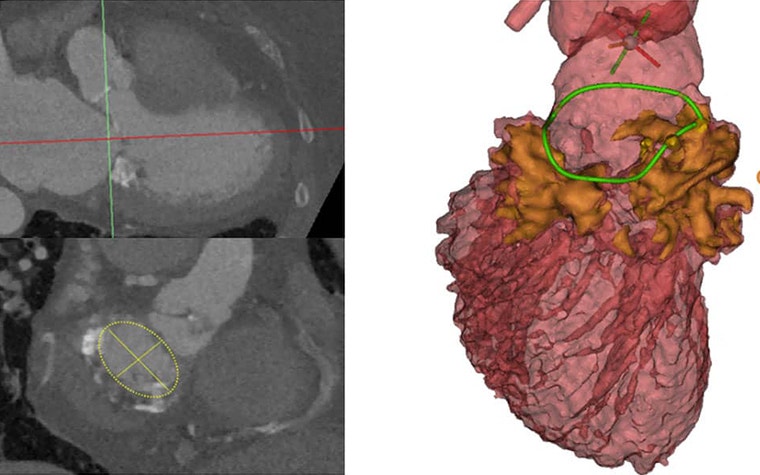
Initially, when they reviewed the CT scans using their 2D planner evaluation methods, they measured the annulus on the 2D slice that visualized it best. Based on their measurements, they believed a 29 mm implant would work for the patient. After uploading the data into Mimics Enlight, they were able to visualize the entire calcification zone, in 3D.
“If you switch around different views, you can get a great image of how the calcium is distributed. Not only the X and the Y planes — but, also in the Z plane, the third dimension. And, by doing measurements in those three planes, we can obtain another kind of measurement of the annulus,” explained Dr. Ooms.
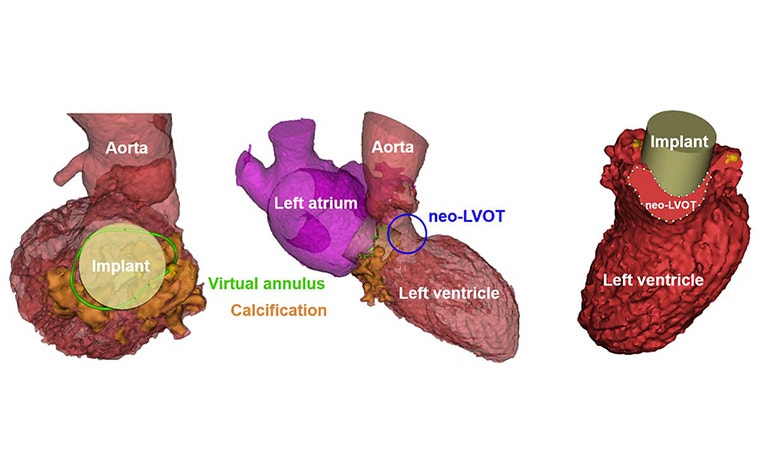
Based on the more detailed visual of where the calcium was and their new measurements, they were able to determine that in fact, a 26 mm valve would be more suitable for the patient. This meant that the valve implant would safely stay in the location that it was implanted. More importantly, the implant would not cause an acute obstruction of the left ventricular outflow tract (LVOT) which means that enough blood can’t flow to the body, including the brain. Obstruction of the LVOT has deadly consequences without emergency surgery.
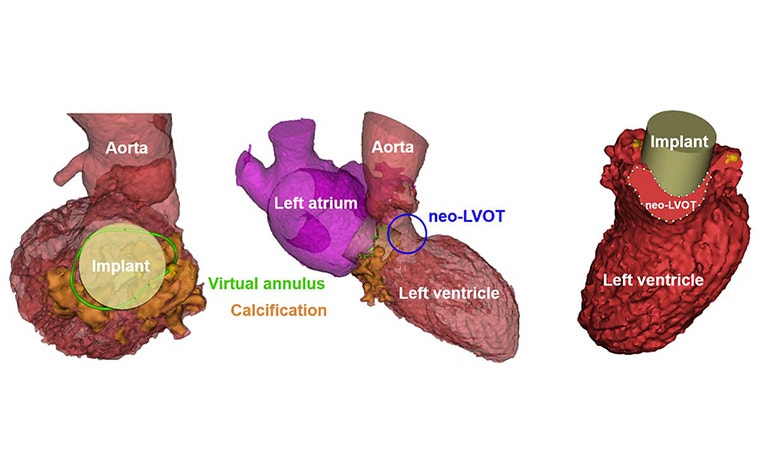
“I think what is crucial is that the anatomical appreciation was different with conventional CT and with 3D planning. We added so much more granularity to our understanding using the 3D planning. And that resulted in a safer approach with less risk of significant complications like obstructing the LVOT due to a neo-LVOT that would have been too small for the patient. Based on the calcium distribution and the 3D appreciation, we realized that a 26 mm would already anchor properly in this case," explained Prof. Van Mieghem.
“The 3D print was also very informative. I think it just underscores the importance of 3D and conversely, the limitations of 2D imaging. Really, it's a different world.”
— Prof. Nicolas Van Mieghem, Interventional Cardiology, Erasmus University Medical Center
Additionally, conventional wisdom is to do an implant in a 20-80 approach which means that 80% of the valve would be protruding in the left ventricle outflow tract, while 20% would be in the left atrium. If the team had gone with that common approach based off their 2D planning, they would have completely blocked the LVOT due to the calcification and the patient would have ended up with severe problems. Due to the 3D planning, they realized that a 60-40 or 40-60 approach would be feasible and still allow for proper anchoring and sealing of the implant.
After planning, they also 3D printed a replica of the patient’s heart to practice the procedure using a 26 mm implant. This gave them a boost of confidence that their planning was accurate. When it came time for the procedure, there were no surprises or complications, and the patient has not been re-admitted post-recovery.
As Prof. Van Mieghem put it, “We believe that 3D planning is now mandatory for TMVR cases. 3D planning takes away some of the insecurities that you will have entering the case. To add to that, I think the 3D print was also very informative. I think it just underscores the importance of 3D — of the three dimensions — and conversely, the limitations of 2D imaging. Really, it's a different world.”
A full report of this TMVR case is published in the European Heart Journal - Case Reports.


Prof. Nicolas Van Mieghem is Professor of Interventional Cardiology in the Department of Interventional Cardiology at the Thoraxcenter, Erasmus Medical Center and Fellow of the European Society of Cardiology. He is a principal investigator and steering committee member in multiple ongoing international trials evaluating various coronary and transcatheter valve technologies. So far, he has published and co-authored approximately 130 scientific papers in peer-reviewed journals.
Dr. Joris Ooms is a PhD candidate in interventional cardiology at the Thoraxcenter of the Erasmus University Medical Center, Rotterdam, The Netherlands. He is involved in multiple research projects for the structural heart program including the implementation of advanced pre-procedural planning methods into clinical practice.
L-101542-01
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
