EXPERT INSIGHT
How to Know if Your Clinical Case Is Appropriate for 3D Printing

In November 2018, the 3D printing Special Interest Group (SIG) of the Radiological Society of North America (RSNA) published guidelines for medical 3D printing, targeted towards point-of-care 3D printing, and which clinical cases it may be appropriate for.
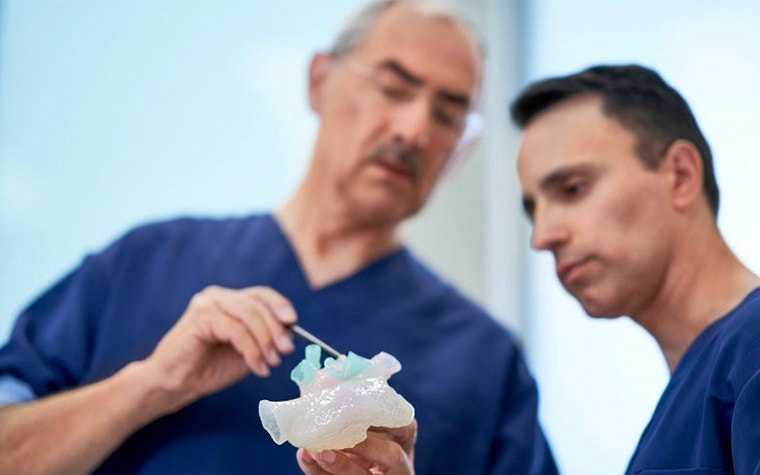
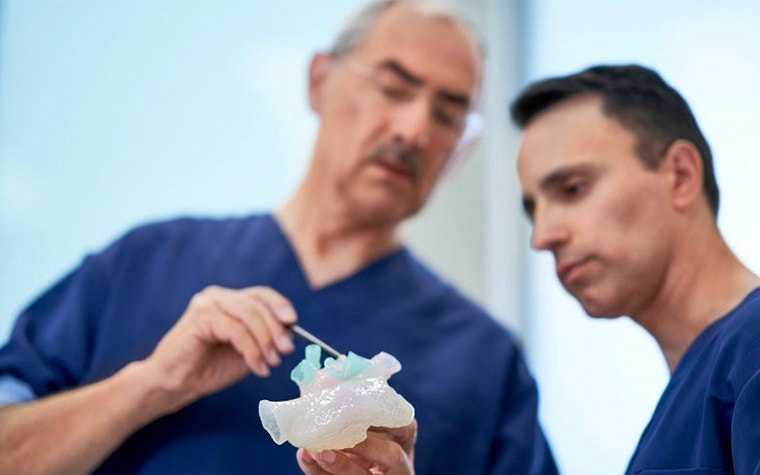
This fits into the SIG’s perspective that “3D printing will play an increasingly important role in enabling precision medicine.” This is backed up by research firm Gartner, which predicts that by 2021, 25% of surgeons will be practicing on 3D-printed models of a patient prior to surgery.


Only by developing standards will there be safe, consistent practices and industry-wide consensus of how and when to use 3D printing. This literature-based guidance document is a giant step forward in that direction.
These guidelines are furthermore influential as they will support new billing codes, called CPT codes, for point-of-care 3D printing, which are due to implemented in July this year. These initial CPT codes make it possible to collect more data on the prevalence of 3D printing and for what cases it is used across U.S. hospitals and will ultimately pave the way for further reimbursement initiatives.
Consistent and safe production of 3D-printed anatomical models
In the guidelines, the SIG recommends the use of FDA-cleared software to 3D print anatomical models. Materialise has cleared two software products to date – namely Mimics inPrint and Mimics Innovation Suite. The unique clearances of Mimics allow the use of certified 3D printers and materials to ensure appropriate quality during the entire medical 3D printing process.
The article outlines how to acquire medical images, for example with appropriate resolution and slice thickness, data prep, material management and quality control among other details on the methodology and 3D printing process.
Is your clinical case appropriate for 3D printing?
The current state of the clinical appropriateness criteria rates three breast conditions, 28 congenital heart disease conditions, 28 craniomaxillofacial conditions, 17 genitourinary conditions, 17 musculoskeletal conditions, and 25 vascular conditions. It describes when it is appropriate to use 3D printing, with the “usually appropriate” classification used for when “data and experience shows an advantage to 3D printing as a method to represent and/or extend the value of data contained in the medical imaging examination.”
Scenarios in this category, in which literature and experts agree 3D printing is most appropriate, include truncus arteriosus, double outlet left ventricle, congenital malformation of skull and facial bones, renal cancer and complex acetabular fracture. The full list of guidelines is an open access publication.
L-100505-01
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
