INTERVIEW
University Hospitals Leuven Consolidates 3D Expertise in a Centralized Point-of-Care Lab
University Hospitals Leuven is Belgium’s largest university hospital and is renowned for its specialized care and innovative treatments. It is also a pioneer in clinical research, helping to drive the future of patient care.
Point-of-care 3D printing wasn’t a new concept for UZ Leuven, but with 3D visualization and printing expertise scattered across its clinical departments, the hospital decided to harness the knowledge and amplify its reach by establishing a centralized lab. The lab, closely linked to the radiology department, brings together the expertise of doctors, scientists, and engineers, and now serves all departments on a project basis.
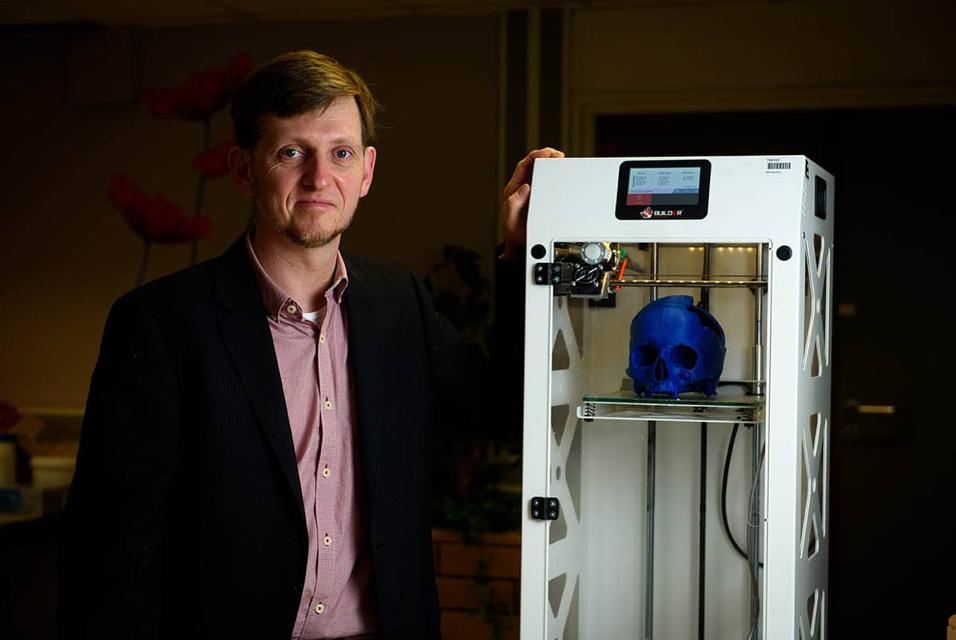
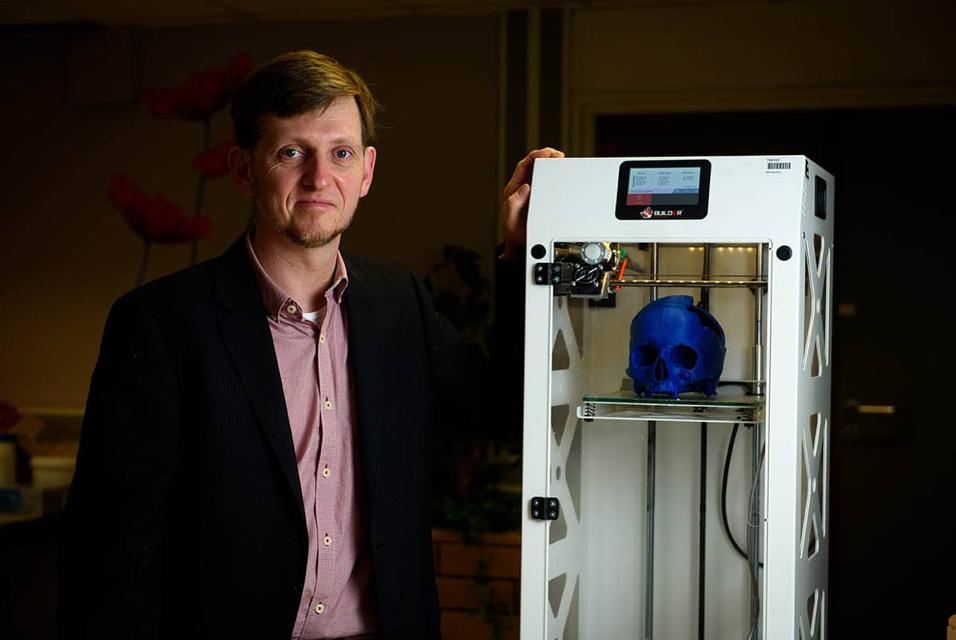
In this article, Prof. Dr. Ir. Stijn De Buck, 3D Point-of-Care Manager, and Prof. Dr. Frank Weekers, Operational Director at UZ Leuven tell us why they decided to consolidate 3D printing efforts, how they planned for success, and what benefits they see in the use of 3D visualization and printing for clinical care, training and education, and research.


What were the main drivers for consolidating 3D printing efforts in UZ Leuven?
Across the hospital, we could see that interest in exploring 3D printing was growing rapidly. Some departments had gone so far as to invest in 3D printing hardware themselves, but with limited internal knowledge and a steep learning curve, they couldn’t use it efficiently.
While other departments were already much more advanced, for example, the radiology department was very proficient in using 3D visualization as part of their diagnostic framework, and the oral and cranio-maxillofacial (CMF) and orthopaedics departments had already built up a wealth of expertise in both 3D printing and visualization.
However, this fragmented landscape meant that the hospital as a whole was far from being able to fully explore the potential that 3D technologies could offer.
We felt that consolidating our efforts in a single, centralized facility would give us the best opportunity to expand our possibilities even further, not only in terms of patient care, but also in the training of medical students and specialists, as well as to support research activities.
Concretely, how did you go about creating a centralized lab?
Identifying and involving all the relevant stakeholders was a key starting point for the whole project. We contacted each clinical department to identify their needs and wishes in terms of 3D printing and visualization. This gave us a realistic picture of the scope of the project and formed the basis for our roadmap.
To structure the project and establish clear roles and responsibilities, we installed a multi-disciplinary steering committee — involving partners from the clinical teams, the imaging departments, the medical and management boards, as well as from the university — who would make key decisions on the priorities for the lab. For example, one of the first decisions we made was to harmonize and centralize the software used throughout the whole hospital.
“We felt that consolidating our efforts in a single, centralized facility would give us the best opportunity to expand our possibilities even further, not only in terms of patient care, but also in the training of medical students and specialists, as well as to support research activities. ”
We also made the decision to closely involve the imaging departments in the new 3D lab. For instance, radiologists and radiology technicians already have a great deal of expertise in interpreting images, and this is often a crucial starting point to accurately segment images, especially for more complex pathologies.
Why did you choose Materialise Mimics ?
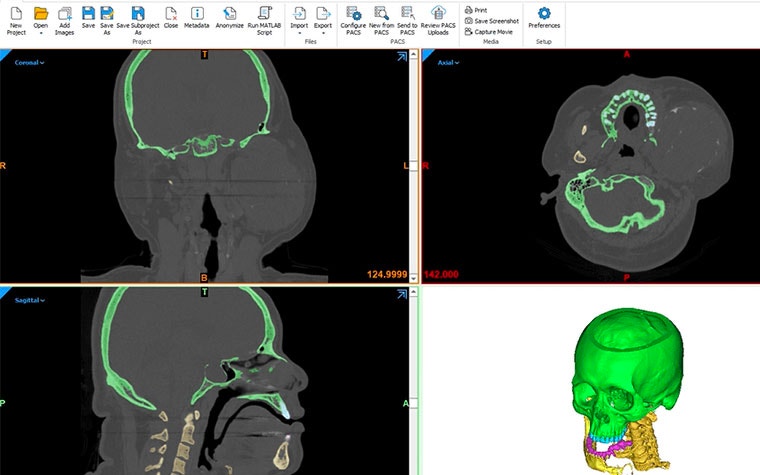
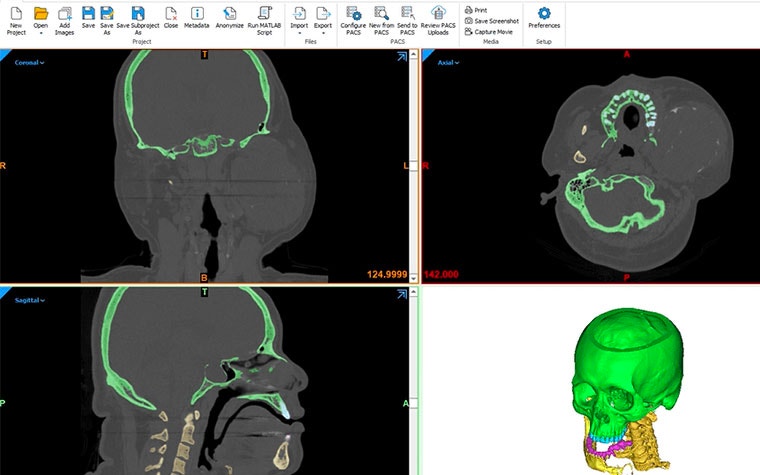
When we compared various software packages on the market, we saw how broad the Mimics package is; it has everything we need to be able to segment images and create 3D models and templates, whether for printing or visualization. The solution includes a number of semi-automated segmentation tools that are practical to use even when dealing with complex pathological anatomy. Furthermore, the software has a multitude of import/export formats and has the necessary tools to interact with (FEM) simulation packages. Also, scripting enables automation of workflows that are used often.
The fact that Mimics is CE-marked medical device software was also important for us, as it means the software complies with medical regulations and we are comfortable using it during clinical routine in addition to its use in our research activities.
On a practical level, being able to manage the software centrally was another key criterion for us, and we feel this brings real benefits, both practically and financially. All clinical departments across the hospital are now using the same software package, which makes the most sense from a training and maintenance perspective.
The training package and individual consultancy that Materialise offered have been particularly appreciated, too. Their flexible approach to rolling out training meant that specific clinical needs and demands of individual departments within the hospital could be taken into account, getting us all off to the best possible start.
How is the 3D printing lab organized today, and how do departments access the technology?
We currently operate on a project basis, with individual departments submitting a request for a specific project to be carried out.
One requirement for using the lab services is that there should already be some clinical evidence that supports the use of 3D printing or visualization for the project. When that’s not available, the project should generate clinical evidence about the suitability of 3D technology for that particular clinical application. In the long term, pursuing measurable clinical evidence gives us a better picture of where the real benefits of 3D printing and/or visualization lie in terms of patient care.
We have also established collaborations with KU Leuven, the university that we are affiliated with, in the context of preclinical research projects.
Where do you see the biggest benefits from using 3D software and printing solutions?
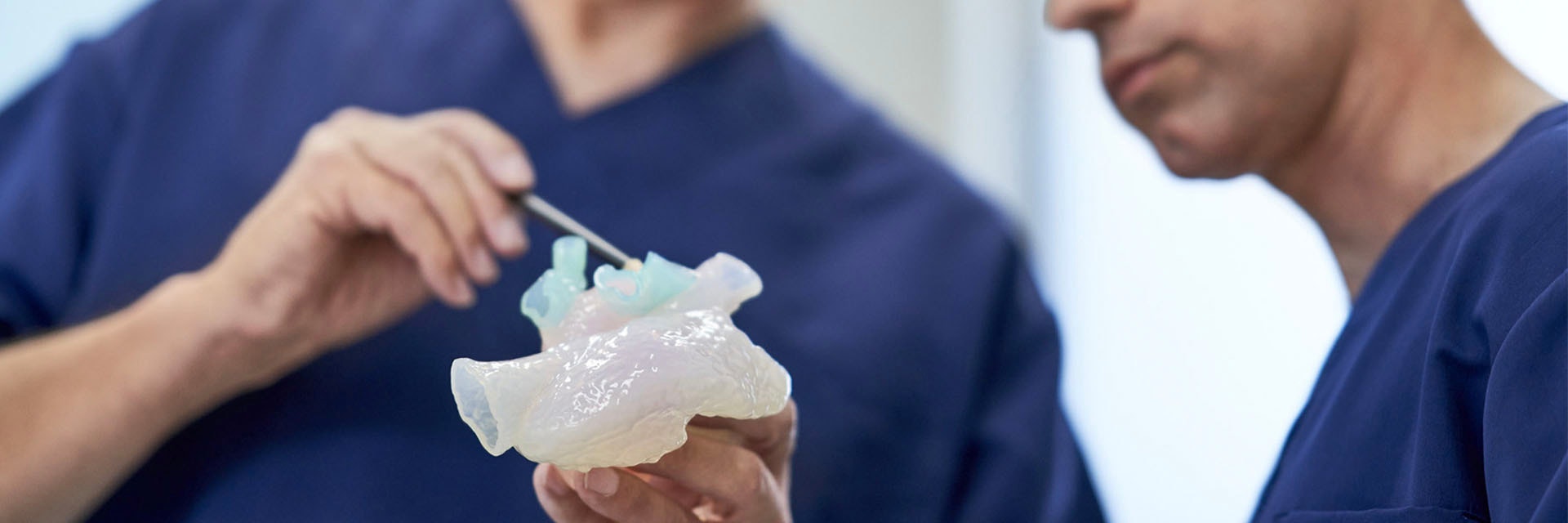
In terms of clinical care, we see several benefits, especially in the case of complex pathologies. Being able to see and explore the anatomy in 3D makes a huge difference to the physician’s understanding. It also means we can plan and even simulate certain procedures before performing them. For example, in complex cardiovascular pathologies, the physician may want to intervene using a catheter. In that case, it’s extremely helpful to be able to visualize the operation site in advance, or even make a 3D print and simulate the intervention.
Another example is orthopaedic surgery to repair complex fractures. Printing a bone like the calcaneus [the large bone forming the heel] allows orthopaedic surgeons to understand the complexity and accurately plan the procedure, thereby reducing operating time and increasing chances of success.
As you can imagine, 3D visualizations, and especially 3D printed models, also greatly improve communication with patients. After all, it’s much easier to understand a physician’s explanations when they can demonstrate on an actual model. This is an aspect where 3D technology can have a really positive impact, as it directly improves the patient experience.
In what other ways is 3D printing adding value for UZ Leuven?
As a university hospital, research — both pre-clinical and clinical — and education are, of course, a big part of what we do. In fact, the three pillars of our strategic plan for 2020 to 2025, ‘Pushing Boundaries,’ are clinical care, research and innovation, and training of medical students and specialists.
3D visualization and printing open a world of opportunity when it comes to research, and we already have some collaborations in place where the lab offers specialized 3D printing solutions for research purposes. The benefits are already clear. With 3D-printed models, taking accurate measurements is much more straightforward, while for simulations, we can now base these on real patient images, resulting in much more accurate and realistic simulations.
When it comes to educating the doctors and specialists of tomorrow, having point-of-care 3D printing contributes in several ways. On the one hand, the lab acts as a knowledge platform that offers the opportunity to learn about 3D printing and its applications. In parallel to this, we have already seen how 3D-printed models can concretely help with training. For example, we already printed a larynx to be used in coniotomy training by the emergency department of the hospital. Students can learn and practice how to insert an intubation tube in the larynx. They can practice this both in adult and child models.
How do you see 3D printing within the hospital evolving in the future?
While we haven’t reached the state of a fully centralized 3D printing facility just yet, we are well on our way, and good communication between departments will help us go even further together. The steering committee, which we already mentioned, plays an important role in facilitating communication. We also created a dedicated internal website that makes the service more accessible.
There’s still a lot of expertise concentrated within the CMF, orthopaedic, and radiotherapy and imaging departments, and by harnessing and sharing this expertise, we will be much stronger in facing the challenges ahead. As our service matures, we also expect to see more examples of crossovers, such as solutions that can work across different departments.
What trends do you expect to see emerge in 3D printing in general?
In the coming years, we expect to see artificial intelligence playing an increasingly important role in automating workflows around personalized 3D visualization and printing, especially in terms of segmentation. This will be a really positive evolution, and it will further increase the potential of this technology. By making it possible to segment more images at a lower cost, truly personalized care will become more affordable.
There will also be great strides made on the hardware side, with printers continuing to evolve, and developments in terms of the materials that can be printed. Who knows when we might even be able to print tissues, or scaffolds that could be used to implant tissue!
It’s clear that there will be some exciting new innovations in the years to come.
For us, establishing our own, centralized point-of-care lab puts us in the driving seat for this exciting journey and ensures we’ll be able to take full advantage of everything that 3D technologies can bring to the future of medicine and personalized care.
L-101660-01
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.