EXPERT INSIGHT
Five Key Takeaways from the Mass Personalization Summit

Events where pioneers — medical device companies, clinicians, and researchers — gather to exchange findings, like at the recent Mass Personalization Summit hosted by Materialise, offer important insight into how personalization will drive business in the near and distant future. Eighty-nine percent of event attendees expect personalized care to become sustainable for many more patients in the coming ten years. The following five key takeaways capture the highlights from the event.
1. Personalization, a catalyst for sustainable patient care
One major concern (and potential for opportunity) detected is whether personalization will truly be sustainable, or just available to outliers or occasional rare cases. When asked about the impact of personalization in ten years, 46% said that it will be sustainable for more common clinical applications. A further 43% said that personalization will be the new standard because it is making healthcare more sustainable. Only 11% believe that personalization will be sustainable mostly for complex or exceptional cases.


Some of the optimism was reflected in Rajit Kamal’s presentation. As the Worldwide President of Sports Medicine and Shoulder Reconstruction for DePuy Synthes, Kamal sees technology as the reason personalization can be achieved with minimal to zero marginal extra cost.
“Think about an iPhone,” said Kamal, “all our iPhones are different. We have different apps. And the cost of doing that is zero. All of us have Netflix, when we login, we see different home accounts with different homepages. It’s personalized to our needs, our viewing behavior. The marginal cost of driving that is zero. That’s what is exciting about technology. I see that same application in orthopaedic surgery.”
2. Medical device companies embrace 3D printing at the point of care
Over 95% of attendees see 3D printing at the point of care as an opportunity instead of a threat because wile 3D printing in a hospital can enable medical device manufacturing in-house, it makes the most sense in specific use cases. This new development is currently being integrated into medical device companies’ product strategies.
A panel discussion, entitled “Personalization: A Key Pillar of Your Business,” with Rajit Kamal, Masha Dumanis from Health Advances, and Michael Librus, Founder and CEO of Synergy elaborated further on the business advantages of personalization at the point of care. Librus, who is helping hospitals with their point-of-care 3D printing activities, says, “We are cooperating with the medical device companies — not competing with them in any way. Medical device companies are coming to us, for example, when a surgeon needs to do a complex revision and they want to do it right and avoid having to do revision for a third time. That is where we are involved: in the planning; the device companies are offering the device, so together we are supporting the needs of the patients and the physicians.”
Kamal continues, “Anything that makes a difference in patient outcomes, that’s our North Star. We will absolutely work with players in the ecosystem to enable that.” But he dismisses point-of-care manufacturing as a threat to medical device companies: “Point-of-care printing has potential. I don’t think it’s for every procedure because you still have to solve questions around cost, quality, consistency of quality, sterilization, etc. I see significant opportunities in complex revisions and complex procedures, and we will absolutely collaborate with partners to enable that for the patients, but I think there will still be room for implants that are not manufactured in the hospital.”


“Point-of-care printing has potential. I don’t think it’s for every procedure because you still have to solve questions around cost, quality, consistency of quality, and sterilization.”
— Rajit Kamal, DePuy Synthes
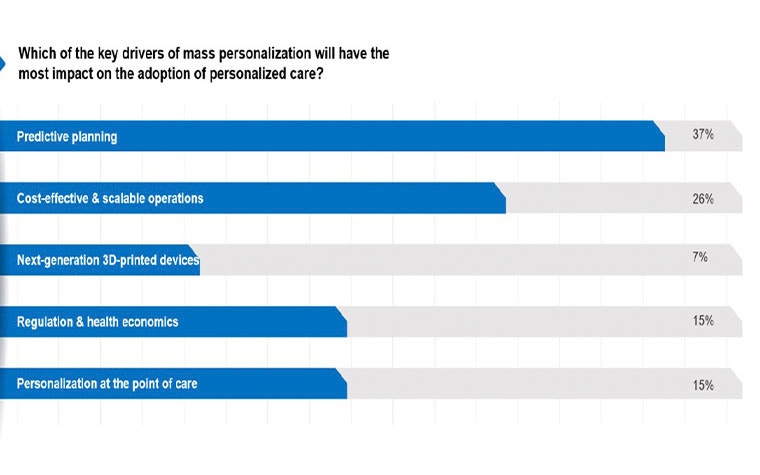
3. Predictive planning is the main driver for mass personalization
The reason behind mass personalization’s impact and growing access centered on five main drivers: predictive planning; cost-effective and scalable operations; next-generation 3D-printed devices; regulation and health economics, and personalization at the point of care.
Interactive polling showed that attendees felt that predictive planning is the main catalyst (37%) behind the widespread adoption of mass personalization, largely because of its ability to effectively transform patient data into a personalized treatment plan that can optimize patient outcomes. Scalable operations came in second with 26%.
Panelists also noted how going from 2D to 3D is significant, specifically in cardiac care. According to Saravana Kumar, CEO of 4C Medical, “If the physician had only the 2D view to look at, he could make any number of mistakes because the interpretation of what is going on inside the heart is affected by what you see.”
To make the point, he showed a slide of Prince William of England making a gesture. From the side view, it was an obscene gesture. From an anterior view, it was the “okay” sign. Kumar believes the same happens in 2D imaging: “The human heart’s left atrium is not the same size and shape in each patient. If we only looked at these in 2D, for example, we would not have the understanding we have today in terms of what to expect anatomically.” He continued, “Our thoughts on how to do planning has to evolve with the improvement on the 3D imaging side, so we give physicians the best idea ahead of time on how to do a cardiovascular procedure with a new device that puts them in a position to succeed — which eventually benefits patients at the end.”
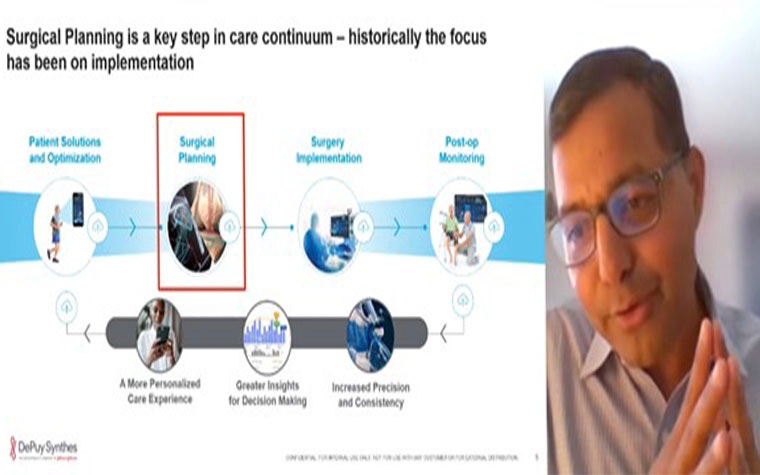
Part of a personalized patient journey should include end-to-end data, which underpins a digital strategy from both hospitals and industry, Rajit Kamal explained. It should lead to a more personalized care experience, give greater insights for decision-making, and increase precision and consistency. Kamal adds, “Surgical planning is a key step in the care continuum starting from the addressing if the patient is the right candidate for surgery. Asking questions like‘which side of care is best suited for the patient?’, ‘what is the right treatment option?’, or ‘is there preoperative readiness?’ is part of creating the individualized care roadmap.
4. Will data, AI, and statistical shape models make humans obsolete?!
Bottom-up technology innovation often promises to disrupt the standard of care, potentially changing the status quo in terms of tasks performed by humans vs. tasks automated by technology.
Just over 70% of the audience agreed with the statement: “In ten years, the use of data, AI, and statistical shape modeling will take over humans’ role when it comes to predictive planning.” But interestingly, the panel of planning experts, consisting of Pras Pathmanathan, Senior Research Scientist at the FDA; Saravana Kumar; and Zihe Zhou, CEO at Zhenyuan Medical, unanimously and firmly disagreed (!) with the conclusion.
An absolute believer in data and modeling, Saravana reminded us that those are all “just tools we use to prepare for the procedure.” He continued that:
“(Technology) does not incorporate the human elements, the nuances of the human body, where you have to anticipate a lot of scenarios. That is why you have to have the human factors, the physicians, the knowledge, the ability to react to situations, which is not always predictable. Data helps you prepare. But I don’t see it replacing what a physician needs to do.”
“Modeling is hard,” said Pathmanathan, “There’s so much complexity in the human body and variation across patients. We see lots of times when people generate models that look promising — and are then asked to validate them with some independent data — and it does not demonstrate the same good results. Or there are too many uncertainties or unknowns. In the near future, there will still be a large human aspect to planning.”
The answer is in the human plus technology combination, says Zhou. “The surgeon can do more mind work, but AI can help at some point, maybe with routine procedures. Humans still will have to decide what to do “because artificial intelligence might make a bad decision if it has incomplete, or incorrect, data.”
“Data helps you prepare. But I don’t see it replacing what a physician needs to do.”
— Saravana Kumar, 4C Medical
5. AI, the super-technology
The debate is still ongoing, but of the technologies that have emerged over the past few years that show enormous potential, AI is seen as the most disruptive technology for personalized care in the coming five to ten years. In part because AI can expand the scope of personalized applications by improving scalability.
The audience’s pronounced belief in artificial intelligence is illustrated below:
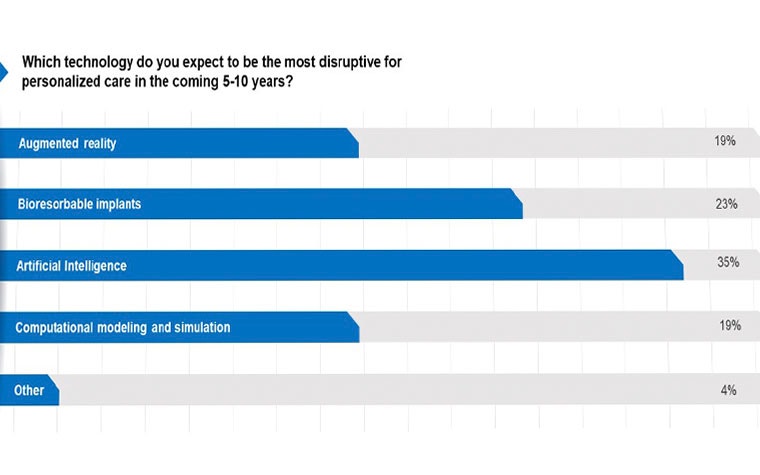


The panel on disruptive innovations, featuring René van Dormolen, Mixed Reality Lead at Microsoft; Pieter Slagmolen, Innovation Manager at Materialise; and Mohit Chhaya, CEO of BellaSeno, all found a reason for artificial intelligence coming on top.
Van Dormolen, a longtime AI aficionado at Microsoft, posited that “empowering all the things that we have seen in this summit: everything is built using AI technology... for visual recognition, for listening to someone speak and interpret, automatic anchoring, the visual overlay of information onto reality — AI is the technology behind these experiences.”
For Chhaya, AI is essential for his company’s additive manufacturing to produce bioresorbable implants, which are 90% porous, but require bonding between layers. BellaSano uses AI to analyze pictures of those layers and understand if they are bonding well. “No clear quality control measure which we can apply on a layer-by-layer basis existed, but we found a great application of AI where we could visually identify well-bonded layers and found a lot of value in terms of safety for the patient and efficiency in manufacturing.”
In the day and age where healthcare costs are increasingly scrutinized, Pieter Slagmolen felt that AI is especially advantageous. “Clearly the reason AI is probably top of the poll is because it is embedded in all the other innovative technologies, as Rene Van Dormolen mentioned, but it’s also important to note the cost-saving benefits. There is a lot of data being generated in healthcare industries. There is probably no better way to manage that data than AI technologies — and at a marginal cost!”
The ultimate winner?
Materialise’s Mass Personalization Summit covered a lot of material, opinions, and innovations. The biggest takeaway was that personalized care will be a sustainable, and a fundamental, part of the future of health. Thinking about it strategically, in terms of data, new technologies are opportunities that will ultimately strengthen healthcare’s body of knowledge, efficiency — and most importantly — patient outcomes.
L-102728-01
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
